J Korean Soc Radiol.
2015 Dec;73(6):408-412. 10.3348/jksr.2015.73.6.408.
Contiguous Spinal Metastasis Mimicking Infectious Spondylodiscitis
- Affiliations
-
- 1Department of Radiology, Hanyang University Hospital, Seoul, Korea. radsh@medimail.co.kr
- 2Department of Pathology, National Police Hospital, Seoul, Korea.
- KMID: 2130948
- DOI: http://doi.org/10.3348/jksr.2015.73.6.408
Abstract
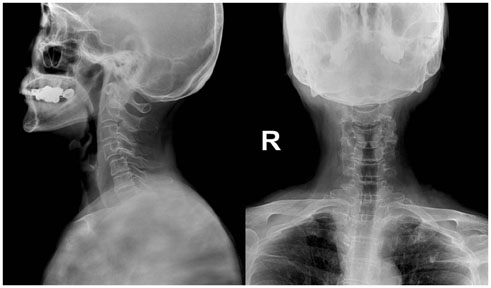
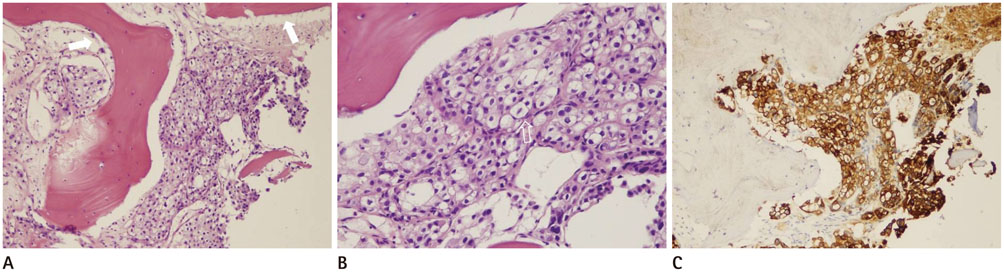
- Differential diagnosis between spinal metastasis and infectious spondylodiscitis is one of the occasional challenges in daily clinical practice. We encountered an unusual case of spinal metastasis in a 75-year-old female breast cancer patient that mimicked infectious spondylodiscitis. Magnetic resonance imaging (MRI) showed diffuse bone marrow infiltrations with paraspinal soft tissue infiltrative changes in 5 contiguous cervical vertebrae without significant compression fracture or cortical destruction. These MRI findings made it difficult to differentiate between spinal metastasis and infectious spondylodiscitis. Infectious spondylodiscitis such as tuberculous spondylodiscitis was regarded as the more appropriate diagnosis due to the continuous involvement of > 5 cervical vertebrae. The patient's clinical presentation also supported the presumptive diagnosis of infectious spondylodiscitis rather than spinal metastasis. Intravenous antibiotics were administered, but clinical symptoms worsened despite treatment. After pathologic confirmation by computed tomography-guided biopsy, we were able to confirm a final diagnosis of spinal metastasis.
MeSH Terms
Figure
Reference
-
1. Resnick D, Kransdorf MJ. Bone and joint imaging. 3rd ed. Philadelphia: Elsevier Saunders;2005. p. 1251–1252.2. Hong SH, Choi JY, Lee JW, Kim NR, Choi JA, Kang HS. MR imaging assessment of the spine: infection or an imitation? Radiographics. 2009; 29:599–612.3. Alcalay M, Azais I, Brigeon B, Babin P, Vandermarcq P, Debiais F, et al. Strategy for identifying primary malignancies with inaugural bone metastases. Rev Rhum Engl Ed. 1995; 62:632–642.4. Brage ME, Simon MA. Evaluation, prognosis, and medical treatment considerations of metastatic bone tumors. Orthopedics. 1992; 15:589–596.5. Shah LM, Salzman KL. Imaging of spinal metastatic disease. Int J Surg Oncol. 2011; 2011:769753.6. Khattry N, Thulkar S, Das A, Khan SA, Bakhshi S. Spinal tuberculosis mimicking malignancy: atypical imaging features. Indian J Pediatr. 2007; 74:297–298.7. Sans N, Faruch M, Lapègue F, Ponsot A, Chiavassa H, Railhac JJ. Infections of the spinal column--spondylodiscitis. Diagn Interv Imaging. 2012; 93:520–529.8. James SL, Davies AM. Imaging of infectious spinal disorders in children and adults. Eur J Radiol. 2006; 58:27–40.9. Gillams AR, Chaddha B, Carter AP. MR appearances of the temporal evolution and resolution of infectious spondylitis. AJR Am J Roentgenol. 1996; 166:903–907.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spondylodiscitis Misdiagnosed as Spinal Stenosis and Compression Fracture: A report of two cases
- Magnetic Resonance Imaging Findings of Early Spondylodiscitis: Interpretive Challenges and Atypical Findings
- Spondylodiscitis after Cervical Nucleoplasty without Any Abnormal Laboratory Findings
- Multiple Non-contiguous Spine Fractures with Concomitant Injuries: A Case Report
- Intramedullary Spinal Cord Metastasis from Breast Cancer Mimicking Delayed Radiation Myelopathy: Detection With 18F-FDG PET/CT