J Korean Soc Radiol.
2015 Dec;73(6):357-366. 10.3348/jksr.2015.73.6.357.
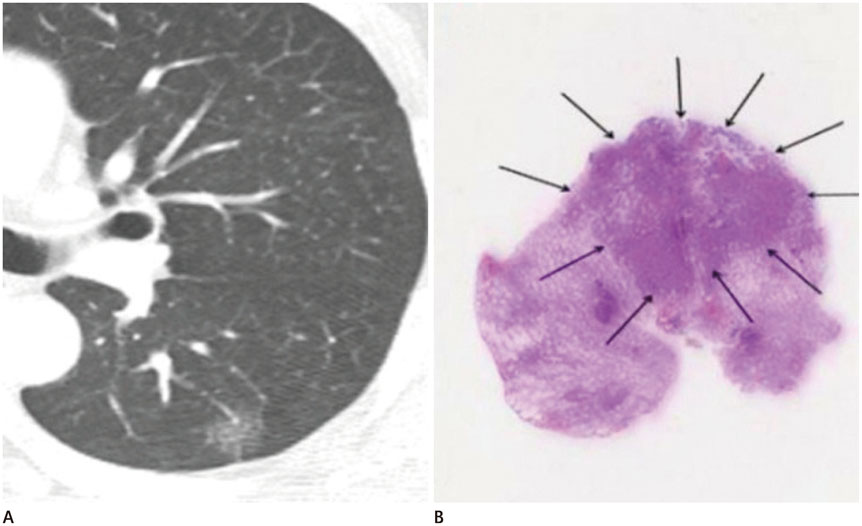
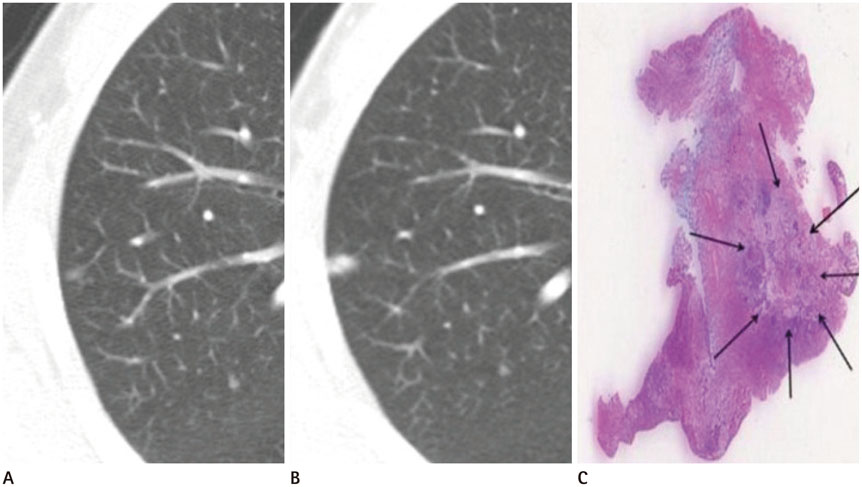
Ground-Glass Nodule on Thin-Section CT: Differentiation among Adenocarcinoma In Situ, Minimally Invasive Adenocarcinoma and Lepidic Predominant Invasive Adenocarcinoma
- Affiliations
-
- 1Department of Radiology, Gangneung Asan Hospital, College of Medicine, University of Ulsan, Gangneung, Korea. ryu@gnah.co.kr
- 2Department of Pathology, Gangneung Asan Hospital, College of Medicine, University of Ulsan, Gangneung, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Gangneung Asan Hospital, College of Medicine, University of Ulsan, Gangneung, Korea.
- KMID: 2130940
- DOI: http://doi.org/10.3348/jksr.2015.73.6.357
Abstract
- PURPOSE
To investigate different computed tomography (CT) features among adenocarcinoma in situ (AIS), minimally invasive adenocarcinoma (MIA), and lepidic predominant invasive adenocarcinoma (LPA) that appeared as ground-glass nodules (GGN). We also analyzed different CT findings between Group A (AIS and MIA) and Group B (LPA).
MATERIALS AND METHODS
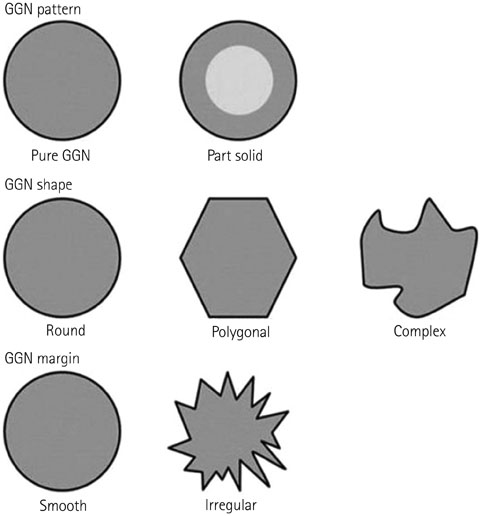
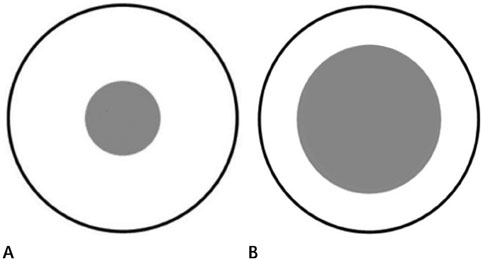
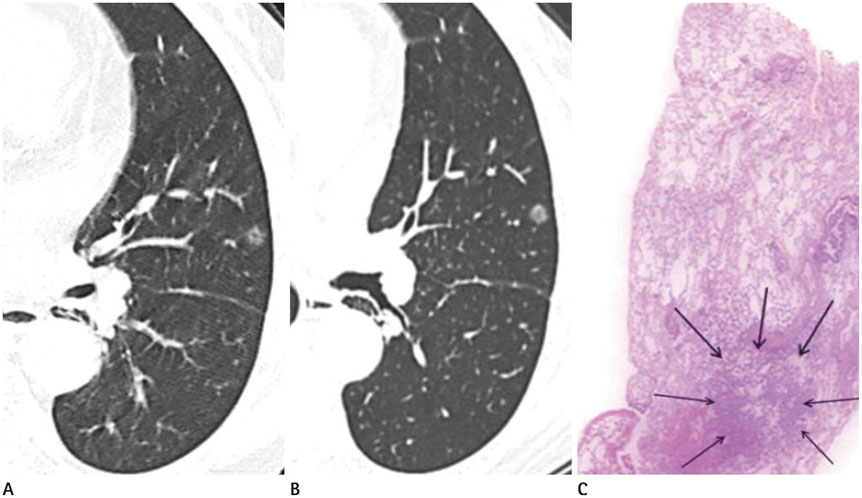
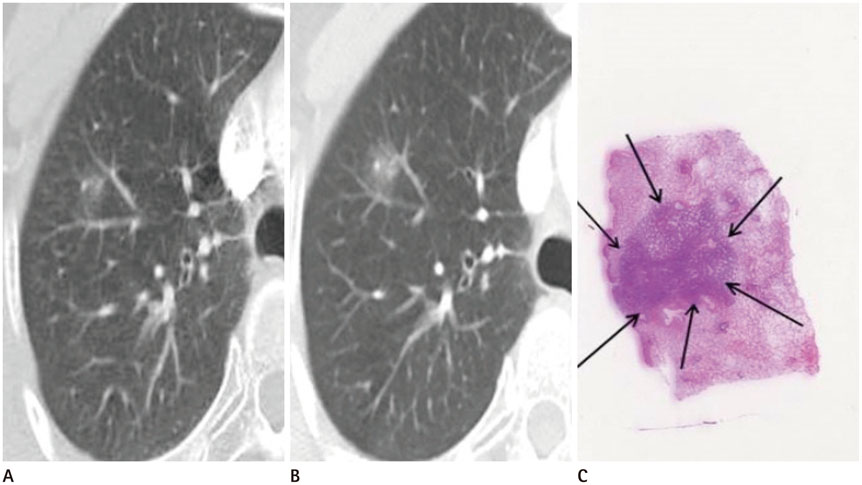
We evaluated 19 AIS, 4 MIA, and 9 LPA images that were histologically confirmed and manifested as GGN on thin-section CT scans. CT scans were assessed for lesion characteristics: size, shape, solid portion, internal air density, marginal irregularity and pleural tag. CT findings of Group A and Group B were analyzed using the Kruskal-Wallis test or Fisher's exact test.
RESULTS
A significant statistical difference was seen between AIS and LPA for lesion characteristics (p < 0.05). No significant difference was observed between AIS and MIA. Round or polygonal shape with smooth margin was significantly associated with Group A, and complex shape with marginal irregularity was associated with Group B.
CONCLUSION
Group A (AIS and MIA) could be distinguished from Group B (LPA) by smaller lesion size, round or polygonal shape, smaller solid portion and smooth margin.
Figure
Reference
-
1. Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011; 6:244–285.2. Lee HJ, Lee CH, Jeong YJ, Chung DH, Goo JM, Park CM, et al. IASLC/ATS/ERS International Multidisciplinary Classification of Lung Adenocarcinoma: novel concepts and radiologic implications. J Thorac Imaging. 2012; 27:340–353.3. Koike T, Togashi K, Shirato T, Sato S, Hirahara H, Sugawara M, et al. Limited resection for noninvasive bronchioloalveolar carcinoma diagnosed by intraoperative pathologic examination. Ann Thorac Surg. 2009; 88:1106–1111.4. Sakurai H, Dobashi Y, Mizutani E, Matsubara H, Suzuki S, Takano K, et al. Bronchioloalveolar carcinoma of the lung 3 centimeters or less in diameter: a prognostic assessment. Ann Thorac Surg. 2004; 78:1728–1733.5. Watanabe S, Watanabe T, Arai K, Kasai T, Haratake J, Urayama H. Results of wedge resection for focal bronchioloalveolar carcinoma showing pure ground-glass attenuation on computed tomography. Ann Thorac Surg. 2002; 73:1071–1075.6. Van Schil PE, Asamura H, Rusch VW, Mitsudomi T, Tsuboi M, Brambilla E, et al. Surgical implications of the new IASLC/ATS/ERS adenocarcinoma classification. Eur Respir J. 2012; 39:478–486.7. Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology. 2013; 268:265–273.8. Li F, Sone S, Abe H, Macmahon H, Doi K. Malignant versus benign nodules at CT screening for lung cancer: comparison of thin-section CT findings. Radiology. 2004; 233:793–798.9. Lee HJ, Goo JM, Lee CH, Park CM, Kim KG, Park EA, et al. Predictive CT findings of malignancy in ground-glass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol. 2009; 19:552–560.10. Ost D, Fein AM, Feinsilver SH. Clinical practice. The solitary pulmonary nodule. N Engl J Med. 2003; 348:2535–2254.11. Colby TV, Noguchi M, Henschke C, Vazquenz MF, Geisinger K, Yokose T, et al. Adenocarinoma. In : Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, editors. World Health Organization Classification of Tumours: Pathology and Genetics, Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press;2003. p. 35–44.12. Goo JM, Park CM, Lee HJ. Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol. 2011; 196:533–543.13. Park CM, Goo JM, Lee HJ, Lee CH, Chun EJ, Im JG. Nodular ground-glass opacity at thin-section CT: histologic correlation and evaluation of change at follow-up. Radiographics. 2007; 27:391–408.14. Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013; 266:304–317.15. Lim HJ, Ahn S, Lee KS, Han J, Shim YM, Woo S, et al. Persistent pure ground-glass opacity lung nodules ≥ 10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest. 2013; 144:1291–1299.16. Lee HJ, Goo JM, Lee CH, Yoo CG, Kim YT, Im JG. Nodular ground-glass opacities on thin-section CT: size change during follow-up and pathological results. Korean J Radiol. 2007; 8:22–31.17. Nakajima R, Yokose T, Kakinuma R, Nagai K, Nishiwaki Y, Ochiai A. Localized pure ground-glass opacity on high-resolution CT: histologic characteristics. J Comput Assist Tomogr. 2002; 26:323–329.18. Lee HY, Choi YL, Lee KS, Han J, Zo JI, Shim YM, et al. Pure ground-glass opacity neoplastic lung nodules: histopathology, imaging, and management. AJR Am J Roentgenol. 2014; 202:W224–W233.19. Park CM, Goo JM, Kim TJ, Lee HJ, Lee KW, Lee CH, et al. Pulmonary nodular ground-glass opacities in patients with extrapulmonary cancers: what is their clinical significance and how can we determine whether they are malignant or benign lesions? Chest. 2008; 133:1402–1409.20. Park CM, Goo JM, Lee HJ, Lee CH, Kim HC, Chung DH, et al. CT findings of atypical adenomatous hyperplasia in the lung. Korean J Radiol. 2006; 7:80–86.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expression of Transforming Growth Factor beta1 and Cadherins in Lung Adenocarcinoma
- Improved Surgical Outcomes of Laparoscopic Gastrectomy Compared with Conventional Open Gastrectomy for Gastric Adenocarcinoma in Obese Patients
- Size of Non-lepidic Invasive Pattern Predicts Recurrence in Pulmonary Mucinous Adenocarcinoma: Morphologic Analysis of 188 Resected Cases with Reappraisal of Invasion Criteria
- Volume and Mass Doubling Time of Lung Adenocarcinoma according to WHO Histologic Classification
- Ground-Glass Opacity in Lung Metastasis from Adenocarcinoma of the Stomach: A Case Report