Korean J Leg Med.
2015 Nov;39(4):127-131. 10.7580/kjlm.2015.39.4.127.
Ludwig's Angina: An Autopsy Case
- Affiliations
-
- 1Forensic Medicine Division, National Forensic Service Gwangju Institute, Jangseong, Korea. pdrdream@gmail.com
- 2Department of Otolaryngology-Head and Neck Surgery, Chonnam National University Medical School, Gwangju, Korea.
- 3Department of Forensic Medicine, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2130857
- DOI: http://doi.org/10.7580/kjlm.2015.39.4.127
Abstract
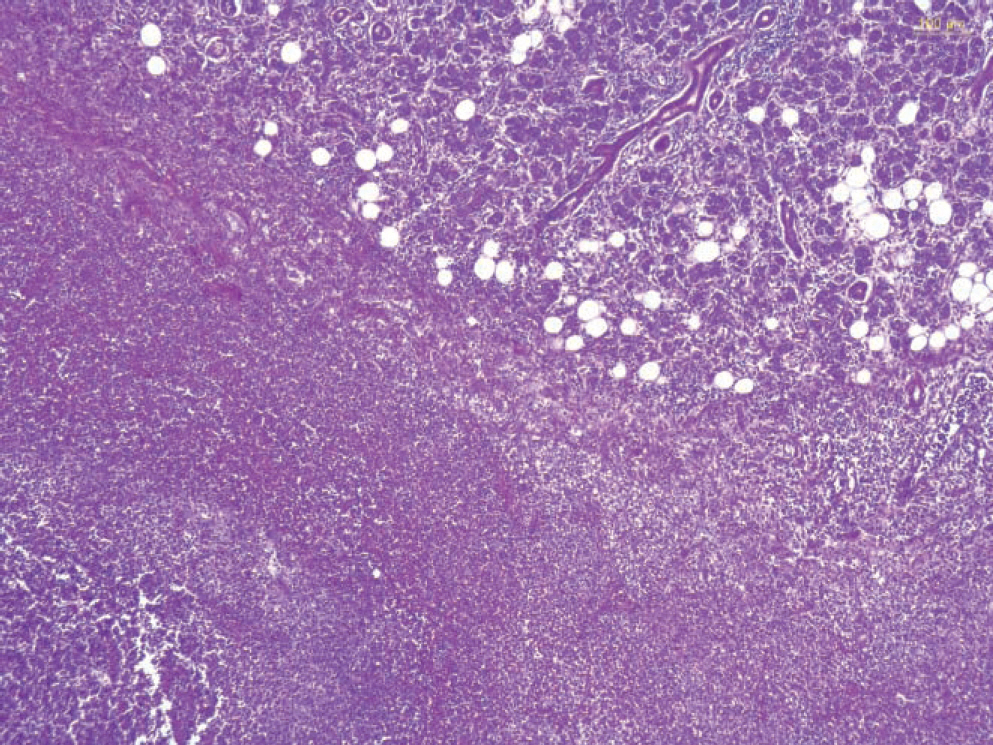
- Ludwig's angina is a progressive gangrenous cellulitis and edema of the soft tissues of the neck and floor of the mouth. Ludwig's angina can be fatal as a result of progressive swelling of the soft tissues of the neck and elevation and posterior displacement of the tongue, resulting in airway obstruction. We report the case of a 77-yearold man who was admitted to the dental hospital with a toothache and headache. He was diagnosed with left submandibular space abscess. Four days post-admission, the submandibular and submental abscess was incised and drained. After the operation, the patient suddenly developed dyspnea and suffered cardiopulmonary arrest and died. An autopsy was performed, and exploration of the neck revealed a submental and submandibular abscess with massive inflammation, edema, and an abscess in multiple layers of the cervical subcutaneous tissue. After autopsy, the cause of death was confirmed as Ludwig's angina with a deep neck abscess. Ludwig's angina is a rapidly progressive cellulitis that often results in death by asphyxia or sepsis and is rarely seen in a forensic autopsy practice. Here in we report a case of Ludwig's angina and present a review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Saifeldeen K, Evans R. Ludwig's angina. Emerg Med J. 2004; 21:242–3.
Article2. Costain N, Marrie TJ. Ludwig's angina. Am J Med. 2011; 124:115–7.
Article3. Bansal A, Miskoff J, Lis RJ. Otolaryngologic critical care. Crit Care Clin. 2003; 19:55–72.
Article4. Kremer MJ, Blair T. Ludwig angina: forewarned is forearmed. AANA J. 2006; 74:445–51.5. Candamourty R, Venkatachalam S, Babu MR, et al. Ludwig's angina: an emergency. A case report with literature review. J Nat Sci Biol Med. 2012; 3:206–8.6. Lee WI, Lee J, Bassed R, et al. Postmortem CT findings in a case of necrotizing cellulitis of the floor of the mouth (Ludwig angina). Forensic Sci Med Pathol. 2014; 10:109–13.
Article7. Marcus BJ, Kaplan J, Collins KA. A case of Ludwig angina: a case report and review of the literature. Am J Forensic Med Pathol. 2008; 29:255–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ludwig Angina
- Sudden Death Due to Undiagnosed Ludwig’s Angina: An Autopsy Case Report
- Air-Q(R)sp-assisted awake fiberoptic bronchoscopic intubation in a patient with Ludwig's angina
- A Case Report of Fatal Mediastinal Abscess Secondary to Odontogenic Infection
- A Case of Hypoxic Encephalopathy Following Anesthesia for a Patient with Ludwig`s Angina