Yonsei Med J.
2014 Jul;55(4):967-974. 10.3349/ymj.2014.55.4.967.
Comparison of Methicillin-Resistant Staphylococcus aureus Community-Acquired and Healthcare-Associated Pneumonia
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Institute of Chest Disease, Yonsei University College of Medicine, Seoul, Korea. STOPYES@yuhs.ac
- 2Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 3Division of Pulmonology, Department of Internal Medicine, Institute of Chest Disease, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea.
- KMID: 2130821
- DOI: http://doi.org/10.3349/ymj.2014.55.4.967
Abstract
- PURPOSE
Methicillin-resistant Staphylococcus aureus (MRSA) is recognized as an important cause of not only healthcare-associated pneumonia (HCAP) but also community-acquired pneumonia (CAP). We determined the impact of MRSA on differences in clinical characteristics, courses, and outcomes between CAP and HCAP.
MATERIALS AND METHODS
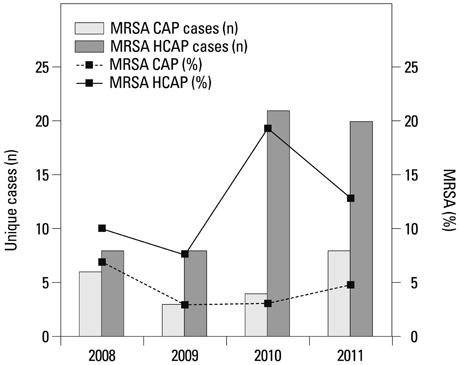
We conducted a retrospective observational study on 78 adult patients admitted with MRSA pneumonia at a university-affiliated tertiary hospital between January 2008 and December 2011. We compared baseline characteristics, chest radiographs, treatment outcomes, and drug resistance patterns between the CAP and HCAP groups.
RESULTS
Of the 78 patients with MRSA pneumonia, 57 (73.1%) were HCAP and 21 (26.9%) were CAP. MRSA infection history in the previous year (29.8% vs. 14.3%, p=0.244) tended to be more common in HCAP than in CAP. Despite similar Pneumonia Severity Index scores (151 in CAP vs. 142 in HCAP), intubation rates (38.1% vs. 17.5%; p=0.072) and intensive care unit admission (42.9% vs. 22.8%; p=0.095) tended to be higher in the CAP group, while 28-day mortality was higher in the HCAP group (14.3% vs. 26.3%; p=0.368), although without statistical significance. All patients showed sensitivity to vancomycin and linezolid; meanwhile, HCAP patients showed greater resistance to gentamicin than CAP patients (58.3% vs. 16.6%; p=0.037). The median total hospital charges were 6899 American dollars for CAP and 5715 American dollars for HCAP (p=0.161).
CONCLUSION
MRSA pneumonia showed significantly differences in baseline characteristics, chest radiographs, treatment outcomes, and medical expenses between HCAP and CAP groups.
Keyword
MeSH Terms
Figure
Reference
-
1. Rubinstein E, Kollef MH, Nathwani D. Pneumonia caused by methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008; 46:Suppl 5. S378–S385.2. Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol. 2013; 34:1–14.
Article3. Park HK, Song JU, Um SW, Koh WJ, Suh GY, Chung MP, et al. Clinical characteristics of health care-associated pneumonia in a Korean teaching hospital. Respir Med. 2010; 104:1729–1735.
Article4. Schreiber MP, Chan CM, Shorr AF. Resistant pathogens in nonnosocomial pneumonia and respiratory failure: is it time to refine the definition of health-care-associated pneumonia? Chest. 2010; 137:1283–1288.
Article5. Shindo Y, Sato S, Maruyama E, Ohashi T, Ogawa M, Hashimoto N, et al. Health-care-associated pneumonia among hospitalized patients in a Japanese community hospital. Chest. 2009; 135:633–640.
Article6. Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, Albrecht V, Limbago B, et al. Prevalence of methicillin-resistant staphylococcus aureus as an etiology of community-acquired pneumonia. Clin Infect Dis. 2012; 54:1126–1133.
Article7. Rello J, Bodi M, Mariscal D, Navarro M, Diaz E, Gallego M, et al. Microbiological testing and outcome of patients with severe community-acquired pneumonia. Chest. 2003; 123:174–180.
Article8. Lobo LJ, Reed KD, Wunderink RG. Expanded clinical presentation of community-acquired methicillin-resistant Staphylococcus aureus pneumonia. Chest. 2010; 138:130–136.
Article9. Kallen AJ, Brunkard J, Moore Z, Budge P, Arnold KE, Fosheim G, et al. Staphylococcus aureus community-acquired pneumonia during the 2006 to 2007 influenza season. Ann Emerg Med. 2009; 53:358–365.
Article10. Gillet Y, Vanhems P, Lina G, Bes M, Vandenesch F, Floret D, et al. Factors predicting mortality in necrotizing community-acquired pneumonia caused by Staphylococcus aureus containing Panton-Valentine leukocidin. Clin Infect Dis. 2007; 45:315–321.
Article11. Hidron AI, Low CE, Honig EG, Blumberg HM. Emergence of community-acquired meticillin-resistant Staphylococcus aureus strain USA300 as a cause of necrotising community-onset pneumonia. Lancet Infect Dis. 2009; 9:384–392.
Article12. Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America for the Treatment of Methicillin-Resistant Staphylococcus aureus Infections in Adults and Children. Clin Infect Dis. 2011; 52:e18–e55.
Article13. Nathwani D, Morgan M, Masterton RG, Dryden M, Cookson BD, French G, et al. Guidelines for UK practice for the diagnosis and management of methicillin-resistant Staphylococcus aureus (MRSA) infections presenting in the community. J Antimicrob Chemother. 2008; 61:976–994.
Article14. Mylotte JM. Nursing home-acquired pneumonia. Clin Infect Dis. 2002; 35:1205–1211.
Article15. Muder RR. Pneumonia in residents of long-term care facilities: epidemiology, etiology, management, and prevention. Am J Med. 1998; 105:319–330.
Article16. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002; 137:791–797.
Article17. Carratalà J, Fernández-Sabé N, Ortega L, Castellsagué X, Rosón B, Dorca J, et al. Outpatient care compared with hospitalization for community-acquired pneumonia: a randomized trial in low-risk patients. Ann Intern Med. 2005; 142:165–172.
Article18. American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005; 171:388–416.19. Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007; 51:3568–3573.
Article20. Murray PR, Washington JA. Microscopic and baceriologic analysis of expectorated sputum. Mayo Clin Proc. 1975; 50:339–344.21. Kim MH, Lee WI, Kang SY. Detection of methicillin-resistant Staphylococcus aureus in healthcare workers using real-time polymerase chain reaction. Yonsei Med J. 2013; 54:1282–1284.
Article22. Defres S, Marwick C, Nathwani D. MRSA as a cause of lung infection including airway infection, community-acquired pneumonia and hospital-acquired pneumonia. Eur Respir J. 2009; 34:1470–1476.
Article23. Carratalà J, Mykietiuk A, Fernández-Sabé N, Suárez C, Dorca J, Verdaguer R, et al. Health care-associated pneumonia requiring hospital admission: epidemiology, antibiotic therapy, and clinical outcomes. Arch Intern Med. 2007; 167:1393–1399.
Article24. Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005; 128:3854–3862.
Article25. Gillet Y, Issartel B, Vanhems P, Fournet JC, Lina G, Bes M, et al. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet. 2002; 359:753–759.
Article26. Hageman JC, Uyeki TM, Francis JS, Jernigan DB, Wheeler JG, Bridges CB, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003-04 influenza season. Emerg Infect Dis. 2006; 12:894–899.
Article27. Gonzalez BE, Hulten KG, Dishop MK, Lamberth LB, Hammerman WA, Mason EO Jr, et al. Pulmonary manifestations in children with invasive community-acquired Staphylococcus aureus infection. Clin Infect Dis. 2005; 41:583–590.
Article28. Shorr AF, Haque N, Taneja C, Zervos M, Lamerato L, Kothari S, et al. Clinical and economic outcomes for patients with health care-associated Staphylococcus aureus pneumonia. J Clin Microbiol. 2010; 48:3258–3262.
Article29. Shallcross LJ, Fragaszy E, Johnson AM, Hayward AC. The role of the Panton-Valentine leucocidin toxin in staphylococcal disease: a systematic review and meta-analysis. Lancet Infect Dis. 2013; 13:43–54.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Community-Acquired Methicillin-Resistant Staphylococcus aureus Pneumonia
- Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA)
- Community-acquired Methicillin-resistant Staphylococcus aureus Bacteremia Complicated by Acute Cholecystitis
- Detection of Multidrug Resistant Patterns and Associated - genes of Methicillin Resistant Staphylococcus aureus ( MRSA ) Isolated from Clinical Specimens
- A statistical analysis of methicillin-resistant staphylococcus aureus