J Korean Med Sci.
2015 Feb;30(2):199-206. 10.3346/jkms.2015.30.2.199.
Association between Objectively Measured Sleep Quality and Obesity in Community-dwelling Adults Aged 80 Years or Older: A Cross-sectional Study
- Affiliations
-
- 1Research Team for Promoting Independence of the Elderly, Tokyo Metropolitan Geriatric Hospital and Institute of Gerontology, Tokyo, Japan. mijiak@tmig.or.jp
- KMID: 2129652
- DOI: http://doi.org/10.3346/jkms.2015.30.2.199
Abstract
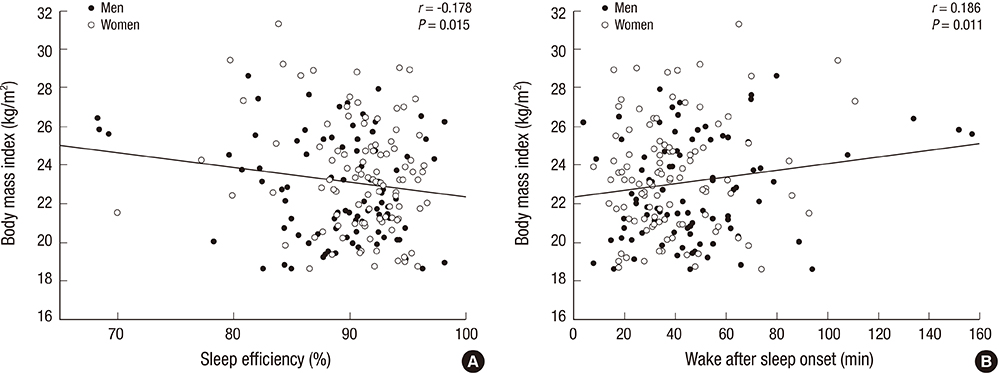
- The purpose of this study was to examine the association between objective measures of sleep quality and obesity in older community-dwelling people. This cross-sectional study included 189 community-dwelling adults aged > or = 80 yr (83.4 +/- 2.5 yr [age range, 80-95 yr]). Participants wore an accelerometer (ActiGraph GT3X+) on their non-dominant wrist 24 hr per day for 7 consecutive nights. Sleep parameters measured included total sleep time, sleep efficiency, and wake after sleep onset (WASO) during the night. Associations between sleep parameters and obesity were investigated by using multivariate logistic regression analysis. In multivariate models, those with sleep efficiency lower than 85% had a 2.85-fold increased odds of obesity, compared with those with sleep efficiency of 85% or higher. Similarly, those with WASO of > or = 60 min (compared with < 60 min) had a 3.13-fold increased odds of obesity. However, there were no significant associations between total sleep time or self-reported napping duration and obesity. We found that poor sleep quality was an independent risk factor for obesity in community-dwelling Japanese adults aged > or = 80 yr, even after controlling for potential confounding factors, including daily physical activity.
Keyword
MeSH Terms
Figure
Reference
-
1. Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005; 13:1849–1863.2. Houston DK, Nicklas BJ, Zizza CA. Weighty concerns: the growing prevalence of obesity among older adults. J Am Diet Assoc. 2009; 109:1886–1895.3. Kim JH, Choi SH, Lim S, Yoon JW, Kang SM, Kim KW, Lim JY, Cho NH, Jang HC. Sarcopenia and obesity: gender-different relationship with functional limitation in older persons. J Korean Med Sci. 2013; 28:1041–1047.4. Al Snih S, Ottenbacher KJ, Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007; 167:774–780.5. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004; 27:1255–1273.6. Akerstedt T, Hume K, Minors D, Waterhouse J. The subjective meaning of good sleep, an intraindividual approach using the Karolinska Sleep Diary. Percept Mot Skills. 1994; 79:287–296.7. Van Cauter E, Leproult R, Plat L. Age-related changes in slow wave sleep and REM sleep and relationship with growth hormone and cortisol levels in healthy men. JAMA. 2000; 284:861–868.8. Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008; 9:S23–S28.9. Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008; 12:289–298.10. Nielsen LS, Danielsen KV, Sørensen TI. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev. 2011; 12:78–92.11. Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB. Self-reported sleep quality is associated with the metabolic syndrome. Sleep. 2007; 30:219–223.12. Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, Chang CJ. The association between self-reported sleep quality and overweight in a Chinese population. Obesity (Silver Spring). 2013; 21:486–492.13. Fogelholm M, Kronholm E, Kukkonen-Harjula K, Partonen T, Partinen M, Härmä M. Sleep-related disturbances and physical inactivity are independently associated with obesity in adults. Int J Obes (Lond). 2007; 31:1713–1721.14. Van Den Berg JF, Van Rooij FJ, Vos H, Tulen JH, Hofman A, Miedema HM, Neven AK, Tiemeier H. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 2008; 17:295–302.15. Kim HK, Suzuki T, Saito K, Yoshida H, Kobayashi H, Kato H, Katayama M. Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc. 2012; 60:16–23.16. Kojima N, Kim H, Saito K, Yoshida H, Yoshida Y, Hirano H, Obuchi S, Shimada H, Suzuki T. Association of knee-extension strength with instrumental activities of daily living in community-dwelling older adults. Geriatr Gerontol Int. 2014; 14:674–680.17. Bassett J. International Diabetes Institute, World Health Organization, Regional Office for the Western Pacific, International Association for the Study of Obesity, International Obesity Task Force. The Asia-Pacific perspective : redefining obesity and its treatment. Australia: Health Communications Australia;2000.18. Matsuzawa Y, Inoue S, Ikeda Y, Sakata T, Saito Y, Satou U, Shirai K, Ohno M, Miyazaki S, Tokunaga K, et al. New diagnostic criteria for obesity and obesity related disorder. J Jpn Soc Study Obes. 2000; 6:18–28.19. Kim M, Kim H. Accuracy of segmental multi-frequency bioelectrical impedance analysis for assessing whole-body and appendicular fat mass and lean soft tissue mass in frail women aged 75 yr and older. Eur J Clin Nutr. 2013; 67:395–400.20. Strath SJ, Pfeiffer KA, Whitt-Glover MC. Accelerometer use with children, older adults, and adults with functional limitations. Med Sci Sports Exerc. 2012; 44:S77–S85.21. Butte NF, Ekelund U, Westerterp KR. Assessing physical activity using wearable monitors: measures of physical activity. Med Sci Sports Exerc. 2012; 44:S5–S12.22. Cellini N, Buman MP, McDevitt EA, Ricker AA, Mednick SC. Direct comparison of two actigraphy devices with polysomnographically recorded naps in healthy young adults. Chronobiol Int. 2013; 30:691–698.23. Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994; 17:201–207.24. Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992; 15:461–469.25. Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011; 43:357–364.26. Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Boudreau R, Cauley JA, Hall M, Matthews KA, Newman AB. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep. 2007; 30:1317–1324.27. Spira AP, Covinsky K, Rebok GW, Punjabi NM, Stone KL, Hillier TA, Ensrud KE, Yaffe K. Poor sleep quality and functional decline in older women. J Am Geriatr Soc. 2012; 60:1092–1098.28. Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005; 28:1289–1296.29. Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA, Lewis CE, Orwoll ES, Stefanick ML, Taylor BC, et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond). 2008; 32:1825–1834.30. van den Berg JF, Knvistingh Neven A, Tulen JH, Hofman A, Witteman JC, Miedema HM, Tiemeier H. Actigraphic sleep duration and fragmentation are related to obesity in the elderly: the Rotterdam Study. Int J Obes (Lond). 2008; 32:1083–1090.31. Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, Liu K. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006; 164:5–16.32. Yan Z, Chang-Quan H, Zhen-Chan L, Bi-Rong D. Association between sleep quality and body mass index among Chinese nonagenarians/centenarians. Age (Dordr). 2012; 34:527–537.33. van den Berg JF, Miedema HM, Tulen JH, Hofman A, Neven AK, Tiemeier H. Sex differences in subjective and actigraphic sleep measures: a population-based study of elderly persons. Sleep. 2009; 32:1367–1375.34. Unruh ML, Redline S, An MW, Buysse DJ, Nieto FJ, Yeh JL, Newman AB. Subjective and objective sleep quality and aging in the sleep heart health study. J Am Geriatr Soc. 2008; 56:1218–1227.35. Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007; 11:163–178.36. Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest. 2010; 137:95–101.37. Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003; 26:342–392.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Comprehensive Health Status and Health-related Quality of Life between Institutionalized Older Adults and Community Dwelling Older Adults
- Sleep Patterns of Older Residents in Long-Term-Care Facilities: A Comparison with Older Adults in Home-Care Services and Community-Dwelling Older Adults
- Effects of Auricular Acupressure Therapy on Psychological Factors, Sleep Quality, and Salivary Cortisol Levels in South Korean Older Adults in the Community: A Single-blind, Randomized Controlled Trial
- Influence of Advance Directives' Self-efficacy of Community-dwelling Older Adults on the Completion of Advance Directives: Mediating the Effect of Intention for Advance Directives: A Cross-Sectional Study
- The Path Model based on Senescent Sleep Model for Sleep in Community-dwelling Older Adults