J Korean Med Sci.
2014 Aug;29(8):1102-1107. 10.3346/jkms.2014.29.8.1102.
Acute Kidney Injury after Using Contrast during Cardiac Catheterization in Children with Heart Disease
- Affiliations
-
- 1Department of Pediatrics, Kyungpook National University School of Medicine, Daegu, Korea. chomh@knu.ac.kr
- 2Joint Institute for Regenerative Medicine, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 2129605
- DOI: http://doi.org/10.3346/jkms.2014.29.8.1102
Abstract
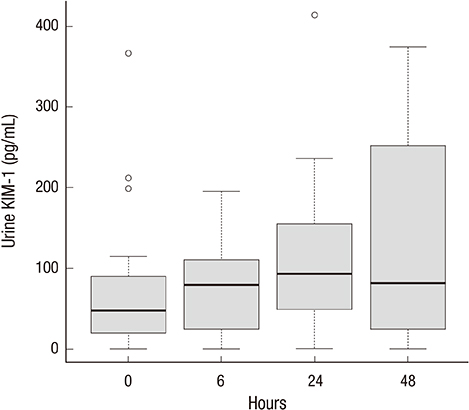
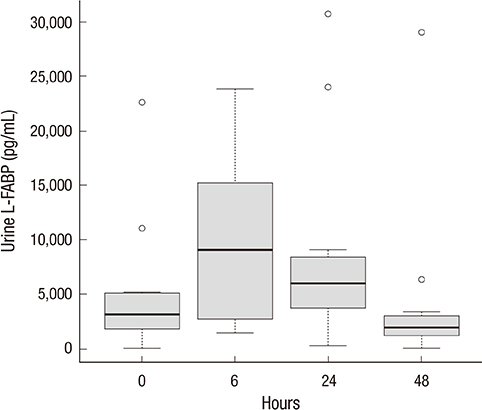
- Acute kidney injury (AKI) is closely associated with the mortality of hospitalized patients and long-term development of chronic kidney disease, especially in children. The purpose of our study was to assess the evidence of contrast-induced AKI after cardiac catheterization in children with heart disease and evaluate the clinical usefulness of candidate biomarkers in AKI. A total of 26 children undergoing cardiac catheterization due to various heart diseases were selected and urine and blood samples were taken at 0 hr, 6 hr, 24 hr, and 48 hr after cardiac catheterization. Until 48 hr after cardiac catheterization, there was no significant increase in serum creatinine level in all patients. Unlike urine kidney injury molecule-1, IL-18 and neutrophil gelatinase-associated lipocalin, urine liver-type fatty acid-binding protein (L-FABP) level showed biphasic pattern and the significant difference in the levels of urine L-FABP between 24 and 48 hr. We suggest that urine L-FABP can be one of the useful biomarkers to detect subclinical AKI developed by the contrast before cardiac surgery.
Keyword
MeSH Terms
-
Acute Kidney Injury/blood/*chemically induced/*urine
Biological Markers/urine
Cardiac Catheterization/*adverse effects
Child
Contrast Media/adverse effects/diagnostic use
Fatty Acid-Binding Proteins/*urine
Female
Heart Defects, Congenital/complications/*radiography
Humans
Iohexol/adverse effects/*analogs & derivatives/diagnostic use
Male
Radiography, Interventional/adverse effects
Reproducibility of Results
Sensitivity and Specificity
Biological Markers
Contrast Media
Fatty Acid-Binding Proteins
Iohexol
Figure
Reference
-
1. Al-Ismaili Z, Palijan A, Zappitelli M. Biomarkers of acute kidney injury in children: discovery, evaluation, and clinical application. Pediatr Nephrol. 2011; 26:29–40.2. Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007; 71:1028–1035.3. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A. Acute Kidney Injury Network. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007; 11:R31.4. Tumlin J, Stacul F, Adam A, Becker CR, Davidson C, Lameire N, McCullough PA. CIN Consensus Working Panel. Pathophysiology of contrast-induced nephropathy. Am J Cardiol. 2006; 98:14K–20K.5. Finn WF. The clinical and renal consequences of contrast-induced nephropathy. Nephrol Dial Transplant. 2006; 21:i2–i10.6. Ronco C, Stacul F, McCullough PA. Subclinical acute kidney injury (AKI) due to iodine-based contrast media. Eur Radiol. 2013; 23:319–323.7. Lenhard DC, Pietsch H, Sieber MA, Ernst R, Lengsfeld P, Ellinghaus P, Jost G. The osmolality of nonionic, iodinated contrast agents as an important factor for renal safety. Invest Radiol. 2012; 47:503–510.8. Ronco C, Kellum JA, Haase M. Subclinical AKI is still AKI. Crit Care. 2012; 16:313.9. Bennett M, Dent CL, Ma Q, Dastrala S, Grenier F, Workman R, Syed H, Ali S, Barasch J, Devarajan P. Urine NGAL predicts severity of acute kidney injury after cardiac surgery: a prospective study. Clin J Am Soc Nephrol. 2008; 3:665–673.10. Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol. 2006; 1:19–32.11. Bianchi P, Carboni G, Pesce G, Isgrò G, Carlucci C, Frigiola A, Giamberti A, Ranucci M. Cardiac catheterization and postoperative acute kidney failure in congenital heart pediatric patients. Anesth Analg. 2013; 117:455–461.12. Devarajan P. Biomarkers for the early detection of acute kidney injury. Curr Opin Pediatr. 2011; 23:194–200.13. Devarajan P. Neutrophil gelatinase-associated lipocalin: an emerging troponin for kidney injury. Nephrol Dial Transplant. 2008; 23:3737–3743.14. Mori K, Lee HT, Rapoport D, Drexler IR, Foster K, Yang J, Schmidt-Ott KM, Chen X, Li JY, Weiss S, et al. Endocytic delivery of lipocalin-siderophore-iron complex rescues the kidney from ischemia-reperfusion injury. J Clin Invest. 2005; 115:610–621.15. Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005; 365:1231–1238.16. Hirsch R, Dent C, Pfriem H, Allen J, Beekman RH 3rd, Ma Q, Dastrala S, Bennett M, Mitsnefes M, Devarajan P. NGAL is an early predictive biomarker of contrast-induced nephropathy in children. Pediatr Nephrol. 2007; 22:2089–2095.17. Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV. Kidney Injury Molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int. 2002; 62:237–244.18. Ichimura T, Bonventre JV, Bailly V, Wei H, Hession CA, Cate RL, Sanicola M. Kidney injury molecule-1 (KIM-1), a putative epithelial cell adhesion molecule containing a novel immunoglobulin domain, is up-regulated in renal cells after injury. J Biol Chem. 1998; 273:4135–4142.19. Liangos O, Perianayagam MC, Vaidya VS, Han WK, Wald R, Tighiouart H, MacKinnon RW, Li L, Balakrishnan VS, Pereira BJ, et al. Urinary N-acetyl-beta-(D)-glucosaminidase activity and kidney injury molecule-1 level are associated with adverse outcomes in acute renal failure. J Am Soc Nephrol. 2007; 18:904–912.20. Han WK, Waikar SS, Johnson A, Betensky RA, Dent CL, Devarajan P, Bonventre JV. Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008; 73:863–869.21. Leslie JA, Meldrum KK. The role of interleukin-18 in renal injury. J Surg Res. 2008; 145:170–175.22. Melnikov VY, Faubel S, Siegmund B, Lucia MS, Ljubanovic D, Edelstein CL. Neutrophil-independent mechanisms of caspase-1- and IL-18-mediated ischemic acute tubular necrosis in mice. J Clin Invest. 2002; 110:1083–1091.23. Parikh CR, Jani A, Mishra J, Ma Q, Kelly C, Barasch J, Edelstein CL, Devarajan P. Urine NGAL and IL-18 are predictive biomarkers for delayed graft function following kidney transplantation. Am J Transplant. 2006; 6:1639–1645.24. Chmurzyńska A. The multigene family of fatty acid-binding proteins (FABPs): function, structure and polymorphism. J Appl Genet. 2006; 47:39–48.25. Wang G, Gong Y, Anderson J, Sun D, Minuk G, Roberts MS, Burczynski FJ. Antioxidative function of L-FABP in L-FABP stably transfected Chang liver cells. Hepatology. 2005; 42:871–879.26. Nakamura T, Sugaya T, Node K, Ueda Y, Koide H. Urinary excretion of liver-type fatty acid-binding protein in contrast medium-induced nephropathy. Am J Kidney Dis. 2006; 47:439–444.27. Negishi K, Noiri E, Doi K, Maeda-Mamiya R, Sugaya T, Portilla D, Fujita T. Monitoring of urinary L-type fatty acid-binding protein predicts histological severity of acute kidney injury. Am J Pathol. 2009; 174:1154–1159.28. Portilla D, Dent C, Sugaya T, Nagothu KK, Kundi I, Moore P, Noiri E, Devarajan P. Liver fatty acid-binding protein as a biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2008; 73:465–472.29. Kato K, Sato N, Yamamoto T, Iwasaki YK, Tanaka K, Mizuno K. Valuable markers for contrast-induced nephropathy in patients undergoing cardiac catheterization. Circ J. 2008; 72:1499–1505.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A clinical study on cardiovascular disease of children taken cardiac catheterization and cineangiography
- Digital subtraction angiography in cardiac disease
- A case of Acute Renal Failure with Hemoglobinuria Following Open Heart Surgery
- Common Atrioventricular Canal Diagnosed by Contrast Echocardiography Report of Two Cases
- The Cause and Treatment of Acute Kidney Injury