Healthc Inform Res.
2015 Jul;21(3):152-160. 10.4258/hir.2015.21.3.152.
Review of Social and Organizational Issues in Health Information Technology
- Affiliations
-
- 1Telfer School of Management, University of Ottawa, Canada. Kuziemsky@telfer.uottawa.ca
- KMID: 2125183
- DOI: http://doi.org/10.4258/hir.2015.21.3.152
Abstract
OBJECTIVES
This paper reviews organizational and social issues (OSIs) in health information technology (HIT).
METHODS
A review and synthesis of the literature on OSIs in HIT was conducted.
RESULTS
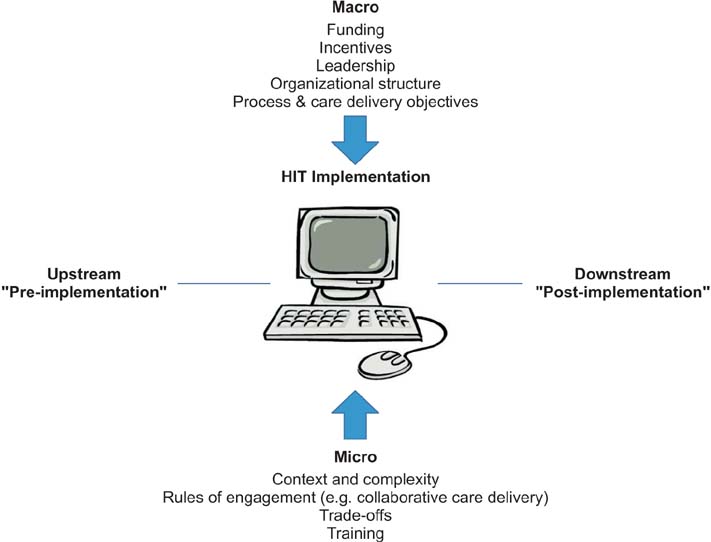
Five overarching themes with respect to OSIs in HIT were identified and discussed: scope and frameworks for defining OSIs in HIT, context matters, process immaturity and complexity, trade-offs will happen and need to be discussed openly, and means of studying OSIs in HIT.
CONCLUSIONS
There is a wide body of literature that provides insight into OSIs in HIT, even if many of the studies are not explicitly labelled as such. The two biggest research needs are more explicit and theoretical studies of OSI in HITs and more research on integrating micro and macro perspectives of HIT use in organizations.
Keyword
MeSH Terms
Figure
Reference
-
1. Institute of Medicine. Health IT and patient safety: building safer systems for better care. Washington (DC): National Academies Press;2012.2. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press;2001.3. Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003; 348(25):2526–2534.
Article4. Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, Burns G, et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc. 2007; 14(1):29–40.
Article5. Coiera E. Building a National Health IT System from the middle out. J Am Med Inform Assoc. 2009; 16(3):271–273.
Article6. Stead WW, Lin HS. Computational technology for effective health care: immediate steps and strategic directions. Washington (DC): National Academies Press;2009.7. Rao S, Brammer C, McKethan A, Buntin MB. Health information technology: transforming chronic disease management and care transitions. Prim Care. 2012; 39(2):327–344.8. McKibbon KA, Lokker C, Handler SM, Dolovich LR, Holbrook AM, O'Reilly D, et al. The effectiveness of integrated health information technologies across the phases of medication management: a systematic review of randomized controlled trials. J Am Med Inform Assoc. 2012; 19(1):22–30.
Article9. Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended sociotechnical consequences of computerized provider order entry. Int J Med Inform. 2007; 76:Suppl 1. S21–S27.
Article10. Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004; 11(2):104–112.
Article11. Borycki E. Trends in health information technology safety: from technology-induced errors to current approaches for ensuring technology safety. Healthc Inform Res. 2013; 19(2):69–78.
Article12. Smith SW, Koppel R. Healthcare information technology's relativity problems: a typology of how patients' physical reality, clinicians' mental models, and healthcare information technology differ. J Am Med Inform Assoc. 2014; 21(1):117–131.
Article13. Agha L. The effects of health information technology on the costs and quality of medical care. J Health Econ. 2014; 34:19–30.
Article14. Coiera E, Aarts J, Kulikowski C. The dangerous decade. J Am Med Inform Assoc. 2012; 19(1):2–5.
Article15. Lluch M. Healthcare professionals' organisational barriers to health information technologies: a literature review. Int J Med Inform. 2011; 80(12):849–862.
Article16. Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. Int J Med Inform. 2013; 82(5):e73–e86.
Article17. Ash J. Organizational factors that influence information technology diffusion in academic health sciences centers. J Am Med Inform Assoc. 1997; 4(2):102–111.
Article18. Lorenzi NM, Riley RT, Blyth AJ, Southon G, Dixon BJ. Antecedents of the people and organizational aspects of medical informatics: review of the literature. J Am Med Inform Assoc. 1997; 4(2):79–93.
Article19. Kaplan B. Addressing organizational issues into the evaluation of medical systems. J Am Med Inform Assoc. 1997; 4(2):94–101.
Article20. Chae YM. Management issues in healthcare information technology. Healthc Inform Res. 2012; 18(2):85–87.
Article21. Yarbrough AK, Smith TB. Technology acceptance among physicians: a new take on TAM. Med Care Res Rev. 2007; 64(6):650–672.22. Rogers EM. Diffusion of innovations. New York (NY): Free Press;1983.23. Karsten R, Schmidt D. Social psychology for IT professionals: a proposed model. Acad Inf Manag Sci. 2004; 8(1):37.24. Bossen C, Jensen LG, Udsen FW. Evaluation of a comprehensive EHR based on the DeLone and McLean model for IS success: approach, results, and success factors. Int J Med Inform. 2013; 82(10):940–953.
Article25. Delone WH, McLean ER. The DeLone and McLean model of information systems success: a ten-year update. J Manag Inf Syst. 2003; 19(4):9–30.
Article26. Kukafka R, Johnson SB, Linfante A, Allegrante JP. Grounding a new information technology implementation framework in behavioral science: a systematic analysis of the literature on IT use. J Biomed Inform. 2003; 36(3):218–227.
Article27. Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005; 293(10):1197–1203.
Article28. Balka E, Doyle-Waters M, Lecznarowicz D, FitzGerald JM. Technology, governance and patient safety: systems issues in technology and patient safety. Int J Med Inform. 2007; 76:Suppl 1. S35–S47.
Article29. Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care: an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007; 14(5):542–549.
Article30. Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform. 2001; 64(2-3):143–156.
Article31. Berg M, Aarts J, van der Lei J. ICT in health care: sociotechnical approaches. Methods Inf Med. 2003; 42(4):297–301.
Article32. Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010; 19:Suppl 3. i68–i74.
Article33. Meeks DW, Takian A, Sittig DF, Singh H, Barber N. Exploring the sociotechnical intersection of patient safety and electronic health record implementation. J Am Med Inform Assoc. 2014; 21(e1):e28–e34.
Article34. Ancker JS, Kern LM, Abramson E, Kaushal R. The Triangle Model for evaluating the effect of health information technology on healthcare quality and safety. J Am Med Inform Assoc. 2012; 19(1):61–65.
Article35. Karsh BT, Weinger MB, Abbott PA, Wears RL. Health information technology: fallacies and sober realities. J Am Med Inform Assoc. 2010; 17(6):617–623.
Article36. Novak L, Brooks J, Gadd C, Anders S, Lorenzi N. Mediating the intersections of organizational routines during the introduction of a health IT system. Eur J Inf Syst. 2012; 21(5):1–31.
Article37. Borycki EM, Kushniruk AW, Bellwood P, Brender J. Technology-induced errors: the current use of frameworks and models from the biomedical and life sciences literatures. Methods Inf Med. 2012; 51(2):95–103.38. Doran D, Haynes BR, Estabrooks CA, Kushniruk A, Dubrowski A, Bajnok I, et al. The role of organizational context and individual nurse characteristics in explaining variation in use of information technologies in evidence based practice. Implement Sci. 2012; 7:122.
Article39. Furukawa MF, King J, Patel V, Hsiao CJ, Adler-Milstein J, Jha AK. Despite substantial progress In EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood). 2014; 33(9):1672–1679.
Article40. Pare G, Raymond L, de Guinea AO, Poba-Nzaou P, Trudel MC, Marsan J, et al. Barriers to organizational adoption of EMR systems in family physician practices: a mixed-methods study in Canada. Int J Med Inform. 2014; 83(8):548–558.
Article41. Villalba-Mora E, Casas I, Lupianez-Villanueva F, Maghiros I. Adoption of health information technologies by physicians for clinical practice: the Andalusian case. Int J Med Inform. 2015; 84(7):477–485.
Article42. Gonen A, Sharon D, Offir A, Lev-Ari L. How to enhance nursing students' intention to use information technology: the first step before integrating it in nursing curriculum. Comput Inform Nurs. 2014; 32(6):286–293.
Article43. Dorr D, Bonner LM, Cohen AN, Shoai RS, Perrin R, Chaney E, et al. Informatics systems to promote improved care for chronic illness: a literature review. J Am Med Inform Assoc. 2007; 14(2):156–163.
Article44. Collins SA, Bakken S, Vawdrey DK, Coiera E, Currie L. Model development for EHR interdisciplinary information exchange of ICU common goals. Int J Med Inform. 2011; 80(8):e141–e149.
Article45. Callen JL, Braithwaite J, Westbrook JI. Contextual implementation model: a framework for assisting clinical information system implementations. J Am Med Inform Assoc. 2008; 15(2):255–262.
Article46. Nash K. Wal-Mart builds supply chain to meet e-commerce demands [Internet]. New York (NY): The Wall Street Journal;c2015. cited at 2015 Jul 10. Available from: http://www.wsj.com/articles/wal-mart-builds-supply-chain-to-meet-e-commerce-demands-1431016708.47. O'Leary KJ, Sehgal NL, Terrell G, Williams MV. High Performance Teams and the Hospital of the Future Project Team. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2012; 7(1):48–54.48. West MA, Lyubovnikova J. Illusions of team working in health care. J Health Organ Manag. 2013; 27(1):134–142.
Article49. Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004; 13:Suppl 1. i85–i90.
Article50. Kuziemsky CE, Varpio L. A model of awareness to enhance our understanding of interprofessional collaborative care delivery and health information system design to support it. Int J Med Inform. 2011; 80(8):e150–e160.
Article51. Reddy MC, Shabot MM, Bradner E. Evaluating collaborative features of critical care systems: a methodological study of information technology in surgical intensive care units. J Biomed Inform. 2008; 41(3):479–487.
Article52. Reddy MC, Spence PR. Collaborative information seeking: a field study of a multidisciplinary patient care team. Inf Process Manag. 2008; 44(1):242–255.
Article53. Kuziemsky CE, Bush P. Coordination considerations of healthcare information technology. Stud Health Technol Inform. 2013; 194:133–138.54. Abraham J, Kannampallil TG, Patel VL. Bridging gaps in handoffs: a continuity of care based approach. J Biomed Inform. 2012; 45:240–254.
Article55. Wong MC, Turner P, Yee KC. Clinical handover improvement in context: exploring tensions between usercentred approaches and standardisation. Stud Health Technol Inform. 2013; 194:48–53.56. Abraham J, Kannampallil T, Patel VL. A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc. 2014; 21(1):154–162.
Article57. Collins SA, Mamykina L, Jordan D, Stein DM, Shine A, Reyfman P, et al. In search of common ground in hand-off documentation in an Intensive Care Unit. J Biomed Inform. 2012; 45(2):307–315.
Article58. Coiera E. Interaction design theory. Int J Med Inform. 2003; 69(2-3):205–222.
Article59. Kannampallil TG, Schauer GF, Cohen T, Patel VL. Considering complexity in healthcare systems. J Biomed Inform. 2011; 44(6):943–947.
Article60. Howard-Grenville JA. The persistence of flexible organizational routines: the role of agency and organizational context. Organ Sci. 2005; 16(6):618–636.
Article61. Braithwaite J, Westbrook J, Iedema R. Restructuring as gratification. J R Soc Med. 2005; 98(12):542–544.
Article62. Bloomrosen M, Starren J, Lorenzi NM, Ash JS, Patel VL, Shortliffe EH. Anticipating and addressing the unintended consequences of health IT and policy: a report from the AMIA 2009 Health Policy Meeting. J Am Med Inform Assoc. 2011; 18(1):82–90.
Article63. Grudin J. Groupware and social dynamics: eight challenges for developers. Commun ACM. 1994; 37(1):92–105.
Article64. Reddy MC, Paul SA, Abraham J, McNeese M, DeFlitch C, Yen J. Challenges to effective crisis management: using information and communication technologies to coordinate emergency medical services and emergency department teams. Int J Med Inform. 2009; 78(4):259–269.
Article65. Campion TR Jr, Waitman LR, Lorenzi NM, May AK, Gadd CS. Barriers and facilitators to the use of computer-based intensive insulin therapy. Int J Med Inform. 2011; 80(12):863–871.
Article66. Vogelsmeier AA, Halbesleben JR, Scott-Cawiezell JR. Technology implementation and workarounds in the nursing home. J Am Med Inform Assoc. 2008; 15(1):114–119.
Article67. McAlearney AS, Hefner JL, Sieck CJ, Huerta TR. The journey through grief: insights from a qualitative study of electronic health record implementation. Health Serv Res. 2015; 50(2):462–488.
Article68. Popovici I, Morita PP, Doran D, Lapinsky S, Morra D, Shier A, et al. Technological aspects of hospital communication challenges: an observational study. Int J Qual Health Care. 2015; 27(3):183–188.
Article69. Kaplan B. Evaluating informatics applications: some alternative approaches: theory, social interactionism, and call for methodological pluralism. Int J Med Inform. 2001; 64(1):39–56.
Article70. Mohammadzadeh N, Safdari R, Rahimi A. Multi-agent system as a new approach to effective chronic heart failure management: key considerations. Healthc Inform Res. 2013; 19(3):162–166.
Article71. Michel-Verkerke MB, Spil TA. The USE IT-adoption-model to predict and evaluate adoption of information and communication technology in healthcare. Methods Inf Med. 2013; 52(6):475–483.
Article72. Zhou Y, Ancker JS, Upadhye M, McGeorge NM, Guarrera TK, Hegde S, et al. The impact of interoperability of electronic health records on ambulatory physician practices: a discrete-event simulation study. Inform Prim Care. 2013; 21(1):21–29.
Article73. Grando MA, Peleg M, Cuggia M, Glasspool D. Patterns for collaborative work in health care teams. Artif Intell Med. 2011; 53(3):139–160.
Article74. Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess. 1998; 2(16):iii–ix. 1–274.
Article75. Kaplan B, Maxwell JA. Qualitative research methods for evaluating computer information systems. In : Anderson JG, Aydin CE, editors. Evaluating the organizational impact of healthcare information systems. New York (NY): Springer;2005. p. 30–55.76. Borycki EM, Househ M, Kushniruk AW, Kuziemsky C. Use of qualitative methods across the software development lifecycle in health informatics. Stud Health Technol Inform. 2011; 164:293–297.77. Strauss AL. Qualitative analysis for social scientists. Cambridge, UK: Cambridge University Press;1987.78. Chiasson M, Reddy M, Kaplan B, Davidson E. Expanding multi-disciplinary approaches to healthcare information technologies: what does information systems offer medical informatics? Int J Med Inform. 2007; 76:Suppl 1. S89–S97.
Article79. Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. J Biomed Inform. 2004; 37(2):128–137.
Article80. Fitzpatrick G, Ellingsen G. A review of 25 years of CSCW research in healthcare: contributions, challenges and future agendas. Comput Support Coop Work. 2013; 22(4-6):609–665.
Article81. Peffers K, Tuunanen T, Rothenberger MA, Chatterjee S. A design science research methodology for information systems research. J Manag Inf Syst. 2007; 24(3):45–77.
Article82. Weng C, McDonald DW, Sparks D, McCoy J, Gennari JH. Participatory design of a collaborative clinical trial protocol writing system. Int J Med Inform. 2007; 76:Suppl 1. S245–S251.
Article83. Peyton L, Kuziemsky C, Langayan D. A case study in interoperable support for collaborative community health-care. Proceedings of the 4th International Workshop on Software Engineering in Health Care (SEHC). 2012 Jun 4-5; Zurich, Switzerland. p. 8–14.84. Filippi L, Spalanzani A. Using technology in an e-learning training course: the role of the student's personal environment. Int J Bus Inf Syst. 2012; 11(1):41–68.
Article85. Orlikowski WJ, Gash DC. Technological frames: making sense of information technology in organizations. ACM Trans Manag Inf Syst. 1994; 12(2):174–207.86. Sadeghi P, Andreev P, Benyoucef M, Momtahan K, Kuziemsky C. Activity theory driven system analysis of complex healthcare processes. Proceedings of the 22nd European Conference on Information Systems (ECIS). 2014 Jun 9-11; Tel Aviv, Israel. p. 1–14.87. Ackerman SL, Tebb K, Stein JC, Frazee BW, Hendey GW, Schmidt LA, et al. Benefit or burden? A sociotechnical analysis of diagnostic computer kiosks in four California hospital emergency departments. Soc Sci Med. 2012; 75(12):2378–2385.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role and mission of the Committee of Health, Korean Medical Association
- Achieving Holistic Health for the Individual through Person-Centered Collaborative Care Supported by Informatics
- The Mediating Effect of Social Capital on the Relationship Between Public Health Managers' Transformational Leadership and Public Health Nurses' Organizational Empowerment in Korea Public Health
- Affecting Factors of Hospital Nurses' Emotional Labor and Social Support on Organizational Commitment
- Methodological Issues in Nursing Research using IT Technology: A Discussion Paper