J Korean Ophthalmol Soc.
2010 Sep;51(9):1276-1281. 10.3341/jkos.2010.51.9.1276.
A Case of Conjunctival Lymphangioma With Clinical Manifestations of Superior Limbic Keratoconjunctivitis After Upper Lid Blepharoplasty
- Affiliations
-
- 1Department of Ophthalmology, KyungHee University School of Medicine, Seoul, Korea. khjinmd@khmc.or.kr
- 2Department of Ophthalmology, Kangwon University School of Medicine, Chuncheon, Korea.
- KMID: 2122297
- DOI: http://doi.org/10.3341/jkos.2010.51.9.1276
Abstract
- PURPOSE
To report a case of conjunctival lymphangioma with clinical manifestations of superior limbic keratoconjunctivitis after upper lid blepharoplasty.
CASE SUMMARY
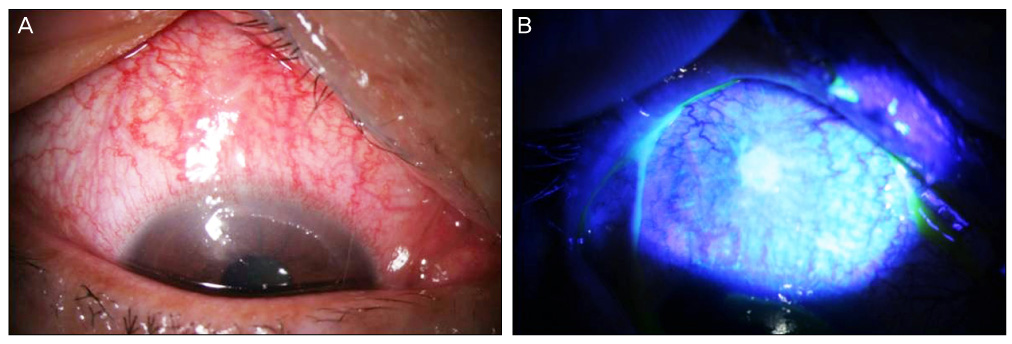
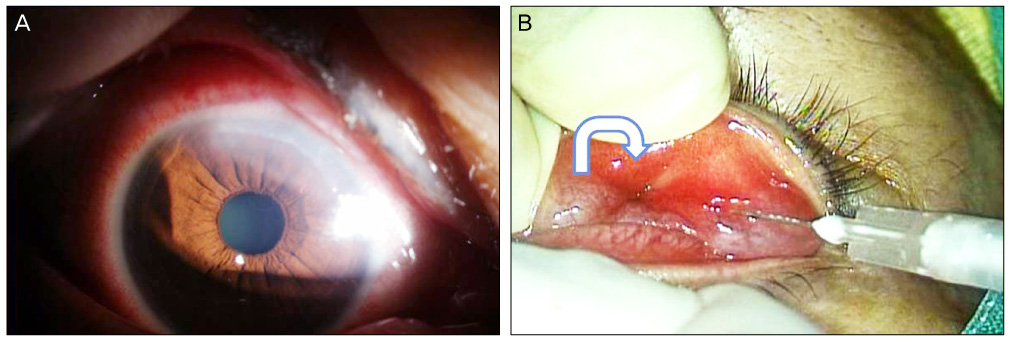
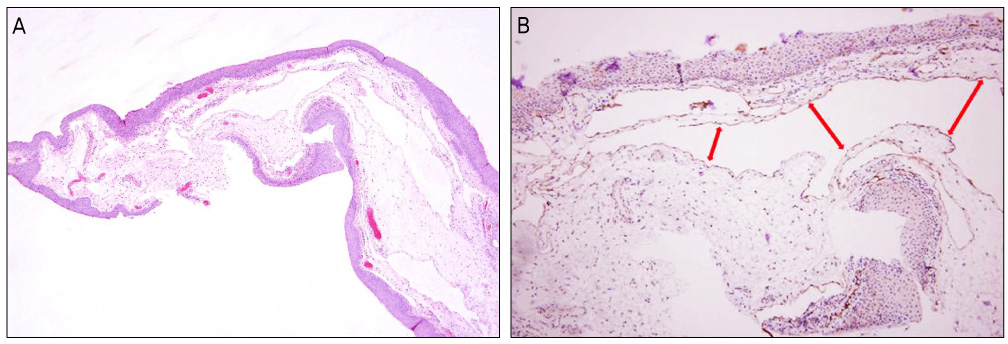
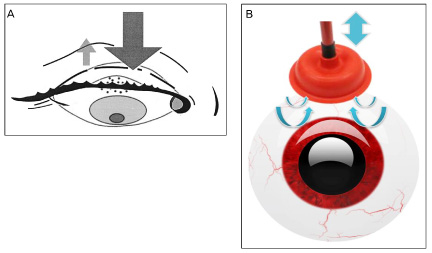
A 55-year-old woman who had upper lid blepharoplasty performed 1 year before complained of pain, injection, and blurred vision in her right eye, which lasted for 2 days. The slit lamp examination revealed a poorly demarcated hypertrophic lesion with central erosion on the superior bulbar conjunctiva and a diffuse corneal erosion and edema in the area of the superior limbus. Tenderness of the superior bulbar conjunctiva and corneal erosion were treated with artificial tears, antibiotic eye drops, and a therapeutic contact lens. Slight anterior chamber reaction was found and treated by steroid eye drops; however, there was no improvement. After eversion of the right upper eyelid with a Desmarres retractor, a hypertrophic lesion with central dimpling was found. However, no exposed sutures were observed. Resection and biopsy of the superior bulbar conjunctiva and a subtarsal triamcinolone injection were performed for diagnosis and treatment. A conjunctival biopsy specimen showed conjunctival lymphangioma.
CONCLUSIONS
Conjunctival lymphangioma can occur due to pressure and friction of an eyelid lesion after upper lid blepharoplasty.
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Isolated Conjunctival Lymphangioma Mimicking a Recurrent Conjunctival Cyst
Jehwi Jeon, Chan Ho Cho, Sang-Bumm Lee
J Korean Ophthalmol Soc. 2018;59(7):676-679. doi: 10.3341/jkos.2018.59.7.676.
Reference
-
1. Kim HB, Kim EW, Lee JB. Superior limbic keratoconjunctivitis. J Korean Ophthalmol Soc. 1981. 22:395–398.2. Nelson JD. Superior limbic keratoconjunctivitis. Eye. 1989. 3:180–189.3. Cher I. Blink-related microtrauma: when the ocular surface harms itself. Clin Experiment Ophthalmol. 2003. 31:183–190.4. Morax S, Touitou V. Complications of blepharoplasty. Orbit. 2006. 25:303–318.5. Kim JT, Kim JH, Kim JC. Visualization of subconjunctival lymphatics and its significance. J Korean Ophthalmol Soc. 2008. 49:1215–1219.6. Singh D. Conjunctival lymphatic system. J Cataract Refract Surg. 2003. 29:632–633.7. Spector JA, Zide BM. Carbon dioxide laser ablation for treatment of lymphangioma of the conjunctiva. Plast Reconstr Surg. 2006. 117:609–612.8. Wiegand S, Eivazi B, Barth PJ, et al. Pathogenesis of lymphangiomas. Virchows Arch. 2008. 453:1–8.9. Theodore FH, Ferry AP. Superior limbic keratoconjunctivitis: clinical and pathological correlations. Arch Ophthalmol. 1970. 84:481–484.10. Cher I. Superior limbic keratoconjunctivitis: multifactorial mechanical pathogenesis. Clin Experiment Ophthalmol. 2000. 28:181–184.11. Sheu MC, Schoenfield L, Jeng BH. Development of superior limbic keratoconjunctivitis after upper eyelid blepharoplasty surgery:support for the mechanical theory of its pathogenesis. Cornea. 2007. 26:490–492.12. Ohashi Y, Watanabe H, Kinoshita S, et al. Vitamin A eyedrops for superior limbic keratoconjunctivitis. Am J Ophthalmol. 1988. 105:523–527.13. Shen YC, Wang CY, Tsai HY, Lee YF. Supratarsal triamcinolone injection in the treatment of superior limbic keratoconjunctivitis. Cornea. 2007. 26:423–426.14. Duke-Elder S. System of Ophthalmology. 1961. Vol. II & VIII. St. Louis: CV Mosby;541–550. 1965;39-46.15. Joo JH, Ko MK, Park MH. Ultrastructural and immunofluorescent features of lymphatic disorders in conjunctiva. J Korean Ophthalmol Soc. 1987. 28:545–550.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Conjunctival Lithiasis with Clinical Manifestations of Superior Limbic Keratoconjunctivitis
- Superior Limbic Keratoconjunctivits
- The Change of Eyebrow Position After Upper Lid Blepharoplasty in Patients With Dermatochalasis
- A Case of Primary Lid Tuberculosis after Upper Lid Blepharoplasty
- Two Cases of Superior Limbic Keratoconjunctivitis Treated with Bevacizumab and Triamcinolone Injection