J Korean Ophthalmol Soc.
2010 Sep;51(9):1250-1257. 10.3341/jkos.2010.51.9.1250.
Glaucoma Diagnostic Performance of Macular and Retinal Nerve Fiber Layer by Spectral-Domain Optical Coherence Tomography
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sungeye@gmail.com
- KMID: 2122293
- DOI: http://doi.org/10.3341/jkos.2010.51.9.1250
Abstract
- PURPOSE
To compare the performance of glaucoma diagnosis according to the macular and peripapillary retinal nerve fiber layer (RNFL) thicknesses, as determined by spectral domain optical coherence tomography (OCT).
METHODS
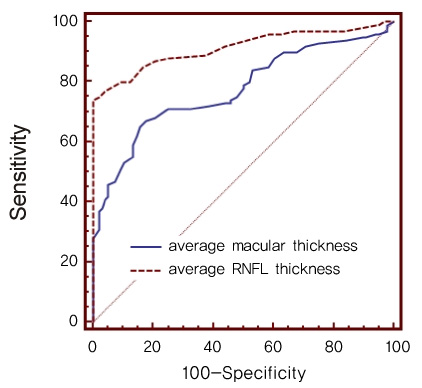
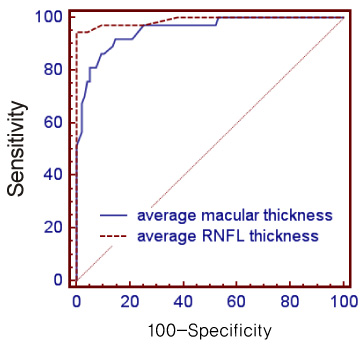
Ninety-six normal, 63 early glaucoma and 37 moderate to advanced glaucomatous eyes were imaged by Cirrus OCT. The areas under the receiver operating characteristics curves (AUCs) of macular and RNFL thicknesses were calculated for discrimination of normal and glaucomatous eyes. The sensitivity and specificity of normative classification of each parameter were assessed.
RESULTS
The glaucoma diagnostic capability determined by AUC was greater when based on the peripapillary RNFL than the macular thickness (0.914, 0.775, p<0.001). Both the early and the moderate-to-advanced group showed higher AUCs in peripapillary RNFL thickness (early glaucoma group; 0.870, 0.670, p<0.001, moderate to advanced glaucoma group; 0.990, 0.954, p=0.03). The inferior outer sector of macular thickness showed highest sensitivity among the parameters (58%).
CONCLUSIONS
Although Cirrus OCT applied to determine macular thickness did not outperform that applied to determine peripapillary RNFL thickness in glaucoma diagnosis, applying Cirrus OCT to determine both thicknesses in diagnosis may help in understanding a patient's status.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Ganglion Cell-Inner Plexiform Layer and Retinal Nerve Fiber Layer after Cataract Surgery
Young Soo Han, Pyung Lee, Kyung Hyun Jin
J Korean Ophthalmol Soc. 2015;56(4):485-493. doi: 10.3341/jkos.2015.56.4.485.
Reference
-
1. Quigley HA, Katz J, Derick RJ, et al. An evaluation of optic disc and nerve fiber layer examinations in monitoring progression of early glaucoma damage. Ophthalmology. 1992. 99:19–28.2. Sommer A, Katz J, Quigley HA, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991. 109:77–83.3. Zeyen TG, Caprioli J. Progression of disc and field damage in early glaucoma. Arch Ophthalmol. 1993. 111:62–65.4. Burgansky-Eliash Z, Wollstein G, Chu T, et al. Optical coherence tomography machine learning classifiers for glaucoma detection: a preliminary study. Invest Ophthalmol Vis Sci. 2005. 46:4147–4152.5. Huang ML, Chen HY. Development and comparison of automated classifiers for glaucoma diagnosis using Stratus optical coherence tomography. Invest Ophthalmol Vis Sci. 2005. 46:4121–4129.6. Kanamori A, Nagai-Kusuhara A, Escano MF, et al. Comparison of confocal scanning laser ophthalmoscopy, scanning laser polarimetry and optical coherence tomography to discriminate ocular hypertension and glaucoma at an early stage. Graefes Arch Clin Exp Ophthalmol. 2006. 244:58–68.7. Lalezary M, Medeiros FA, Weinreb RN, et al. Baseline optical coherence tomography predicts the development of glaucomatous change in glaucoma suspects. Am J Ophthalmol. 2006. 142:576–582.8. Leung CK, Chan WM, Yung WH, et al. Comparison of macular and peripapillary measurements for the detection of glaucoma: an optical coherence tomography study. Ophthalmology. 2005. 112:391–400.9. Manassakorn A, Nouri-Mahdavi K, Caprioli J. Comparison of retinal nerve fiber layer thickness and optic disk algorithms with optical coherence tomography to detect glaucoma. Am J Ophthalmol. 2006. 141:105–115.10. Medeiros FA, Zangwill LM, Bowd C, et al. Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. Am J Ophthalmol. 2005. 139:44–55.11. Naithani P, Sihota R, Sony P, et al. Evaluation of optical coherence tomography and heidelberg retinal tomography parameters in detecting early and moderate glaucoma. Invest Ophthalmol Vis Sci. 2007. 48:3138–3145.12. Nouri-Mahdavi K, Nikkhou K, Hoffman DC, et al. Detection of early glaucoma with optical coherence tomography (StratusOCT). J Glaucoma. 2008. 17:183–188.13. Parikh RS, Parikh S, Sekhar GC, et al. Diagnostic capability of optical coherence tomography (Stratus OCT 3) in early glaucoma. Ophthalmology. 2007. 114:2238–2343.14. Sihota R, Sony P, Gupta V, et al. Comparing glaucomatous optic neuropathy in primary open angle and chronic primary angle closure glaucoma eyes by optical coherence tomography. Ophthalmic Physiol Opt. 2005. 25:408–415.15. Ojima T, Tanabe T, Hangai M, et al. Measurement of retinal nerve fiber layer thickness and macular volume for glaucoma detection using optical coherence tomography. Jpn J Ophthalmol. 2007. 51:197–203.16. Tan O, Li G, Lu AT, et al. Mapping of macular substructures with optical coherence tomography for glaucoma diagnosis. Ophthalmology. 2008. 115:949–956.17. Ishikawa H, Stein DM, Wollstein G, et al. Macular segmentation with optical coherence tomography. Invest Ophthalmol Vis Sci. 2005. 46:2012–2017.18. Zeimer R, Asrani S, Zou S, et al. Quantitative detection of glaucomatous damage at the posterior pole by retinal thickness mapping. A pilot study. Ophthalmology. 1998. 105:224–231.19. Greenfield DS, Bagga H, Knighton RW. Macular thickness changes in glaucomatous optic neuropathy detected using optical coherence tomography. Arch Ophthalmol. 2003. 121:41–46.20. Park SB, Sung KR, Kang SY, et al. Comparison of glaucoma diagnostic capabilities of Cirrus HD and Stratus optical coherence tomography. Arch Ophthalmol. 2009. 127:1603–1609.21. Hodapp E, Parrish RK II, Anderson DR. Clinical decisions in glaucoma. 1993. St Louis: The CV Mosby Co;52–61.22. Mills RP, Budenz DL, Lee PP, et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol. 2006. 141:24–30.23. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988. 44:837–845.24. Wollstein G, Ishikawa H, Wang J, et al. Comparison of three optical coherence tomography scanning areas for detection of glaucomatous damage. Am J Ophthalmol. 2005. 139:39–43.25. Budenz DL, Michael A, Chang RT, et al. Sensitivity and specificity of the Stratus OCT for perimetric glaucoma. Ophthalmology. 2005. 112:3–9.26. Bows C, Zangwill LM, Berry CC, et al. Detecting early glaucoma by assessment of retinal nerve fiber layer thickness and visual function. Invest Ophthalmol Vis Sci. 2001. 42:1993–2003.27. Han K, Jun RM, Choi K. Comparison of RNFL Thickness Measured by Two Different Kind of OCT in NTG Patients. J Korean Ophthalmol Soc. 2009. 12:1853–1859.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thickness of the Macula, Retinal Nerve Fiber Layer, and Ganglion Cell-inner Plexiform Layer in the Macular Hole: The Repeatability Study of Spectral-domain Optical Coherence Tomography
- Choroidal Thickness in Primary Open-Angle Glaucoma Using Spectral-Domain Optical Coherence Tomography
- Clinical Usefulness of Spectral-Domain Optical Coherence Tomography in Glaucoma and NAION
- Spectral-Domain Optical Coherence Tomography Findings in Acute Central Retinal Artery Occlusion
- Retinal Nerve Fiber Layer Thickness Measured with Two Different Spectral Domain Optical Coherence Tomography Devices