Brain Tumor Res Treat.
2015 Oct;3(2):108-114. 10.14791/btrt.2015.3.2.108.
The Efficacy of Postoperative Chemotherapy for Patients with Metastatic Brain Tumors from Non-Small Cell Lung Cancer
- Affiliations
-
- 1Neuro-Oncology Clinic, Center for Specific Organs Cancer, National Cancer Center Hospital, Goyang, Korea. heonyoo@ncc.re.kr
- 2Biometric Research Branch, National Cancer Center Hospital, National Cancer Center, Goyang, Korea.
- KMID: 2114656
- DOI: http://doi.org/10.14791/btrt.2015.3.2.108
Abstract
- BACKGROUND
The purpose of this study is to evaluate the effect of postoperative chemotherapy on recurrence and survival in patients after resection of metastatic brain tumors from non-small cell lung cancers.
METHODS
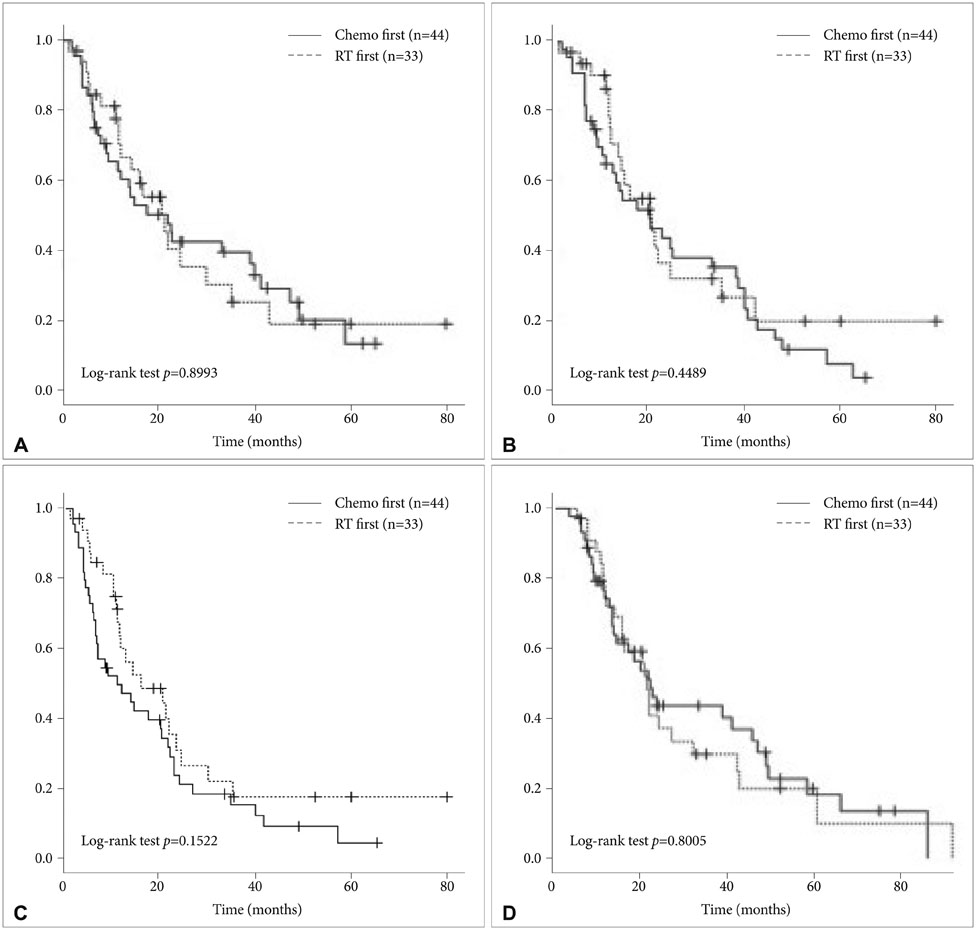
Patients who went through resection of a single metastatic brain tumor from non-small cell lung cancer from July 2001 to December 2012 were reviewed. Those selected were 77 patients who survived more than 3 months after surgery were selected. Among them, 44 patients received various postoperative systemic chemotherapies, 33 patients received postoperative adjuvant whole brain radiotherapy (WBRT). Local/distant recurrence rate, local/distant recurrence free survival, disease free survival (DFS), and overall survival were compared between the two groups.
RESULTS
Among the 77 patients, there were 19 (24.7%) local recurrences. Local recurrence occurred in 7 (21.2%) of 33 patients in the adjuvant radiotherapy (RT) group and in 12 (27.3%) of the 44 patients in the chemotherapy group (p=0.542). Among the 77 patients, there were 34 (44.1%) distant recurrences. Distant recurrence occurred in 7 (21.2%) of the 33 patients in the adjuvant RT group and in 27 (61.4%) of the 44 patients in the chemotherapy group (p<0.0005). Patients' survival in terms of local recurrence free survival, distant recurrence free survival, DFS, and overall survival was not shown to be statistically different between the two groups before and after adjusting for covariates.
CONCLUSION
There was no significant difference observed between postoperative adjuvant chemotherapy and adjuvant WBRT in terms of patients' survival. Postoperative chemotherapy is more feasible and may be an appropriate option for simultaneous control of both primary and metastatic lesions.
Keyword
MeSH Terms
Figure
Reference
-
1. Gaspar LE, Mehta MP, Patchell RA, et al. The role of whole brain radiation therapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010; 96:17–32.
Article2. Sheehan JP, Sun MH, Kondziolka D, Flickinger J, Lunsford LD. Radiosurgery for non-small cell lung carcinoma metastatic to the brain: long-term outcomes and prognostic factors influencing patient survival time and local tumor control. J Neurosurg. 2002; 97:1276–1281.
Article3. Bartolotti M, Franceschi E, Brandes AA. EGF receptor tyrosine kinase inhibitors in the treatment of brain metastases from non-small-cell lung cancer. Expert Rev Anticancer Ther. 2012; 12:1429–1435.
Article4. Lee DH, Han JY, Kim HT, et al. Primary chemotherapy for newly diagnosed nonsmall cell lung cancer patients with synchronous brain metastases compared with whole-brain radiotherapy administered first: result of a randomized pilot study. Cancer. 2008; 113:143–149.
Article5. Yoo H, Kim YZ, Nam BH, et al. Reduced local recurrence of a single brain metastasis through microscopic total resection. J Neurosurg. 2009; 110:730–736.
Article6. Robinet G, Thomas P, Breton JL, et al. Results of a phase III study of early versus delayed whole brain radiotherapy with concurrent cisplatin and vinorelbine combination in inoperable brain metastasis of non-small-cell lung cancer: Groupe Français de Pneumo-Cancérologie (GFPC) Protocol 95-1. Ann Oncol. 2001; 12:59–67.
Article7. Ceresoli GL, Cappuzzo F, Gregorc V, Bartolini S, Crinò L, Villa E. Gefitinib in patients with brain metastases from non-small-cell lung cancer: a prospective trial. Ann Oncol. 2004; 15:1042–1047.
Article8. Chiu CH, Tsai CM, Chen YM, Chiang SC, Liou JL, Perng RP. Gefitinib is active in patients with brain metastases from non-small cell lung cancer and response is related to skin toxicity. Lung Cancer. 2005; 47:129–138.
Article9. Hotta K, Kiura K, Ueoka H, et al. Effect of gefitinib ('Iressa', ZD1839) on brain metastases in patients with advanced non-small-cell lung cancer. Lung Cancer. 2004; 46:255–261.
Article10. Lee DH, Han JY, Lee HG, et al. Gefitinib as a first-line therapy of advanced or metastatic adenocarcinoma of the lung in never-smokers. Clin Cancer Res. 2005; 11:3032–3037.
Article11. Shimato S, Mitsudomi T, Kosaka T, et al. EGFR mutations in patients with brain metastases from lung cancer: association with the efficacy of gefitinib. Neuro Oncol. 2006; 8:137–144.
Article12. Wu C, Li YL, Wang ZM, Li Z, Zhang TX, Wei Z. Gefitinib as palliative therapy for lung adenocarcinoma metastatic to the brain. Lung Cancer. 2007; 57:359–364.
Article13. Kim JE, Lee DH, Choi Y, et al. Epidermal growth factor receptor tyrosine kinase inhibitors as a first-line therapy for never-smokers with adenocarcinoma of the lung having asymptomatic synchronous brain metastasis. Lung Cancer. 2009; 65:351–354.
Article14. Porta R, Sánchez-Torres JM, Paz-Ares L, et al. Brain metastases from lung cancer responding to erlotinib: the importance of EGFR mutation. Eur Respir J. 2011; 37:624–631.
Article15. Grommes C, Oxnard GR, Kris MG, et al. "Pulsatile" high-dose weekly erlotinib for CNS metastases from EGFR mutant non-small cell lung cancer. Neuro Oncol. 2011; 13:1364–1369.
Article16. Armstrong JG, Wronski M, Galicich J, Arbit E, Leibel SA, Burt M. Postoperative radiation for lung cancer metastatic to the brain. J Clin Oncol. 1994; 12:2340–2344.
Article17. Hagen NA, Cirrincione C, Thaler HT, DeAngelis LM. The role of radiation therapy following resection of single brain metastasis from melanoma. Neurology. 1990; 40:158–160.
Article18. Skibber JM, Soong SJ, Austin L, Balch CM, Sawaya RE. Cranial irradiation after surgical excision of brain metastases in melanoma patients. Ann Surg Oncol. 1996; 3:118–123.
Article19. McPherson CM, Suki D, Feiz-Erfan I, et al. Adjuvant whole-brain radiation therapy after surgical resection of single brain metastases. Neuro Oncol. 2010; 12:711–719.
Article20. Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA. 1998; 280:1485–1489.21. Brem S, Meyers CA, Palmer G, Booth-Jones M, Jain S, Ewend MG. Preservation of neurocognitive function and local control of 1 to 3 brain metastases treated with surgery and carmustine wafers. Cancer. 2013; 119:3830–3838.
Article22. Yoo H, Nam BH, Yang HS, Shin SH, Lee JS, Lee SH. Growth rates of metastatic brain tumors in nonsmall cell lung cancer. Cancer. 2008; 113:1043–1047.
Article23. Yoo H, Jung E, Nam BH, et al. Growth rate of newly developed metastatic brain tumors after thoracotomy in patients with non-small cell lung cancer. Lung Cancer. 2011; 71:205–208.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adjuvant Chemotherapy for Completely Resected Non-Small Cell Lung Cancer
- A Case of Metastatic Gastric Cancer Resulting from Small Cell Lung Cancer
- Intussusception induced by jejunal metastasis from non-small cell lung cancer
- Small Cell Lung Cancer at Subcarina Presenting as a Metastatic Brain Tumor
- An Unusual Case of Metastatic Non-Small Cell Lung Cancer Misidentified as Anaplastic Thyroid Cancer