Brain Tumor Res Treat.
2015 Oct;3(2):103-107. 10.14791/btrt.2015.3.2.103.
Long-Term Results of Gamma Knife Radiosurgery for Intracranial Meningioma
- Affiliations
-
- 1Department of Neurosurgery, Yonsei Gamma Knife Center, Yonsei University College of Medicine, Seoul, Korea. changws0716@yuhs.ac
- KMID: 2114655
- DOI: http://doi.org/10.14791/btrt.2015.3.2.103
Abstract
- BACKGROUND
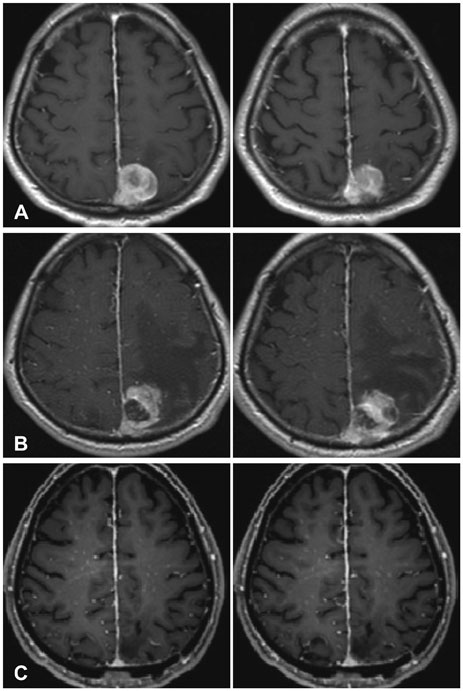
The predominant treatment modality for meningioma is surgical resection. However, gamma knife radiosurgery is also an important treatment modality for meningioma that is small or cannot be completely removed because of its location. In this study, we evaluated the effectiveness and long-term results of radiosurgical treatment for meningioma in our institution.
METHODS
We studied 628 patients (130 men and 498 women) who underwent gamma knife radiosurgery for intracranial meningioma, which is radiologically diagnosed, from Jan 2008 to Nov 2012. We included patients with single lesion meningioma, and followed up after 6 months with imaging, and then at 24 months with a clinical examination. Patients with high-grade meningioma or multiple meningiomas were excluded. We analyzed each of the factors associated with progression free survival. The median patient's age was 56.8 years. Maximal dosage was 27.8 Gy and marginal dosage was 13.9 Gy.
RESULTS
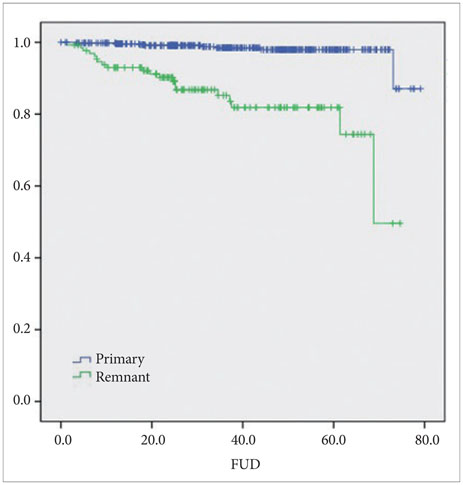
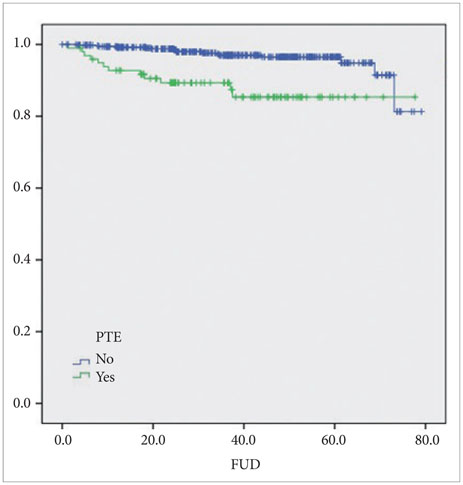
The overall tumor control rate was 95%. Twenty-eight patients (4.4%) showed evidence of tumor recurrence. Ninety-eight patients (15%) developed peritumoral edema (PTE) after gamma-knife surgery; two of them (2%) underwent surgical resections due to PTE. Nine patients had craniotomy and tumor removal after gamma knife surgery.
CONCLUSION
Gamma knife surgery for intracranial meningioma has proven to be a safe and effective treatment tool with successful long-term outcomes. Gamma knife radiosurgery can be especially effective in cases of remnant meningioma after surgical resection or where PTE is not present.
Keyword
Figure
Reference
-
1. Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM. Epidemiology of intracranial meningioma. Neurosurgery. 2005; 57:1088–1095. discussion 1088-95
Article2. Sanna M, Bacciu A, Falcioni M, Taibah A, Piazza P. Surgical management of jugular foramen meningiomas: a series of 13 cases and review of the literature. Laryngoscope. 2007; 117:1710–1719.
Article3. Voss NF, Vrionis FD, Heilman CB, Robertson JH. Meningiomas of the cerebellopontine angle. Surg Neurol. 2000; 53:439–446. discussion 446-7
Article4. Lee JY, Niranjan A, McInerney J, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery providing long-term tumor control of cavernous sinus meningiomas. J Neurosurg. 2002; 97:65–72.
Article5. Pollock BE, Stafford SL. Results of stereotactic radiosurgery for patients with imaging defined cavernous sinus meningiomas. Int J Radiat Oncol Biol Phys. 2005; 62:1427–1431.
Article6. Kreil W, Luggin J, Fuchs I, Weigl V, Eustacchio S, Papaefthymiou G. Long term experience of gamma knife radiosurgery for benign skull base meningiomas. J Neurol Neurosurg Psychiatry. 2005; 76:1425–1430.
Article7. Nicolato A, Foroni R, Alessandrini F, Bricolo A, Gerosa M. Radiosurgical treatment of cavernous sinus meningiomas: experience with 122 treated patients. Neurosurgery. 2002; 51:1153–1159. discussion 1159-61
Article8. Starke RM, Nguyen JH, Rainey J, et al. Gamma Knife surgery of meningiomas located in the posterior fossa: factors predictive of outcome and remission. J Neurosurg. 2011; 114:1399–1409.
Article9. Subach BR, Lunsford LD, Kondziolka D, Maitz AH, Flickinger JC. Management of petroclival meningiomas by stereotactic radiosurgery. Neurosurgery. 1998; 42:437–443. discussion 443-510. Iwai Y, Yamanaka K, Ikeda H. Gamma Knife radiosurgery for skull base meningioma: long-term results of low-dose treatment. J Neurosurg. 2008; 109:804–810.
Article11. DiBiase SJ, Kwok Y, Yovino S, et al. Factors predicting local tumor control after gamma knife stereotactic radiosurgery for benign intracranial meningiomas. Int J Radiat Oncol Biol Phys. 2004; 60:1515–1519.
Article12. Pendl G, Schröttner O, Eustacchio S, Ganz JC, Feichtinger K. Cavernous sinus meningiomas--what is the strategy: upfront or adjuvant gamma knife surgery? Stereotact Funct Neurosurg. 1998; 70:Suppl 1. 33–40.
Article13. Nicolato A, Foroni R, Pellegrino M, et al. Gamma knife radiosurgery in meningiomas of the posterior fossa. Experience with 62 treated lesions. Minim Invasive Neurosurg. 2001; 44:211–217.
Article14. Shin M, Kurita H, Sasaki T, et al. Analysis of treatment outcome after stereotactic radiosurgery for cavernous sinus meningiomas. J Neurosurg. 2001; 95:435–439.
Article15. Roche PH, Pellet W, Fuentes S, Thomassin JM, Régis J. Gamma knife radiosurgical management of petroclival meningiomas results and indications. Acta Neurochir (Wien). 2003; 145:883–888. discussion 888
Article16. Kondziolka D, Patel AD, Kano H, Flickinger JC, Lunsford LD. Long-term Outcomes After Gamma Knife Radiosurgery for Meningiomas. Am J Clin Oncol. 2014; 04. 21. [Epub].
Article17. Flickinger JC, Kondziolka D, Maitz AH, Lunsford LD. Gamma knife radiosurgery of imaging-diagnosed intracranial meningioma. Int J Radiat Oncol Biol Phys. 2003; 56:801–806.
Article18. Bledsoe JM, Link MJ, Stafford SL, Park PJ, Pollock BE. Radiosurgery for large-volume (> 10 cm3) benign meningiomas. J Neurosurg. 2010; 112:951–956.19. Han JH, Kim DG, Chung HT, et al. Gamma knife radiosurgery for skull base meningiomas: long-term radiologic and clinical outcome. Int J Radiat Oncol Biol Phys. 2008; 72:1324–1332.
Article20. Couldwell WT, Cole CD, Al-Mefty O. Patterns of skull base meningioma progression after failed radiosurgery. J Neurosurg. 2007; 106:30–35.
Article21. Goodwin JW, Crowley J, Eyre HJ, Stafford B, Jaeckle KA, Townsend JJ. A phase II evaluation of tamoxifen in unresectable or refractory meningiomas: a Southwest Oncology Group study. J Neurooncol. 1993; 15:75–77.
Article22. Pollock BE, Stafford SL, Link MJ, Garces YI, Foote RL. Single-fraction radiosurgery for presumed intracranial meningiomas: efficacy and complications from a 22-year experience. Int J Radiat Oncol Biol Phys. 2012; 83:1414–1418.
Article23. Jääskeläinen J, Haltia M, Servo A. Atypical and anaplastic meningiomas: radiology, surgery, radiotherapy, and outcome. Surg Neurol. 1986; 25:233–242.
Article24. Modha A, Gutin PH. Diagnosis and treatment of atypical and anaplastic meningiomas: a review. Neurosurgery. 2005; 57:538–550. discussion 538-50
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Exponential growth of an asymptomatic meningioma responsive to fractionated Gamma Knife radiosurgery
- A case of cerebral infarction caused by occlusive vasculopathy after previous gamma knife radiosurgery for pituitary adenoma
- Normal pressure hydrocephalus after gamma knife radiosurgery in a patient with vestibular schwannoma
- Deep Sylvian Meningioma: Case Report
- Long-term Follow-up Results of Gamma Knife Radiosurgery for Benign Tumors Involving Cavernous Sinus