Brain Tumor Res Treat.
2015 Oct;3(2):68-74. 10.14791/btrt.2015.3.2.68.
Treatment Strategy of Intracranial Hemangiopericytoma
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea. jhyun@catholic.ac.kr
- 2Department of Neurosurgery, St. Vincent's Hospital, The Catholic University of Korea, Suwon, Korea.
- KMID: 2114650
- DOI: http://doi.org/10.14791/btrt.2015.3.2.68
Abstract
- BACKGROUND
Recent studies suggest aggressive management combining a grossly total resection (GTR) with adjuvant radiotherapy (RT) as a treatment of choice for intracranial hemangiopericytoma (HPC). However, in these papers, the definitions of complete or GTR are equivocal. In the present study, we reviewed the relevant cases from our experience focused on the clinical efficacy of surgical grading of resection, and analyzed the optimal treatment strategies as well.
METHODS
From January 1995 through December 2014, 17 patients treated for intracranial HPC were included in this study. We analyzed clinical presentation, radiologic appearance, pathologic diagnosis, extent of resection, and follow-up outcomes.
RESULTS
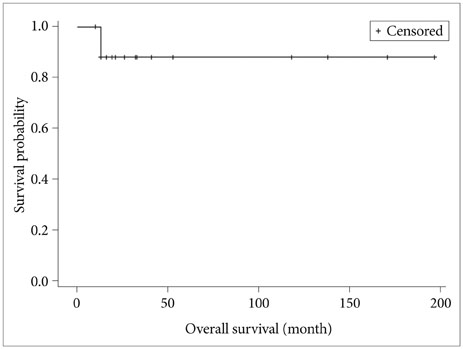
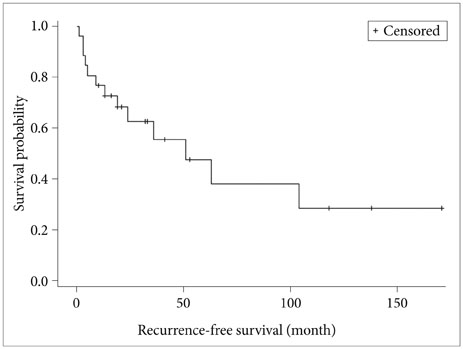
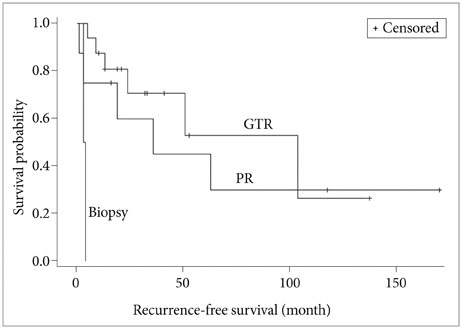
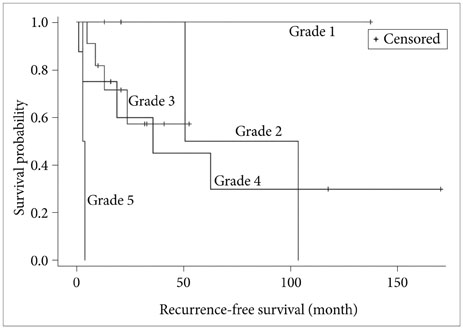
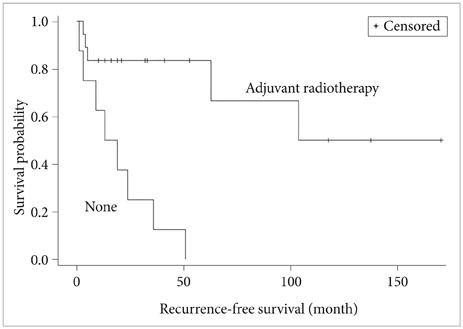
A total of 26 operations were performed including 9 recurrent intracranial HPCs. Every tumor was single and had no evidence of metastasis. Most common area of tumor was parasagittal (8 patients, 47.1%), which is adjoined to superior sagittal sinus. For the initial operation, GTR was performed in 16 cases (61.5%), partial resection (PR) in 8 cases (30.8%), and an endoscopic biopsy in 2 patients (7.7%). In Simpson grading system, grade 1 was done in 2 patients (7.7%), grade 2 in 11 patients (42.3%) and grade 3 in 3 patients (11.5%). Postoperative RT was delivered in 16 patients (94.1%) regardless of the extent of resection. The median 57.57 Gy (range, 50-60 Gy) was delivered in median 33 fractions (range, 30-40). The extent of resection (conventional classification and Simpson grading system) and adjuvant RT were significantly associated with recurrence-free survival.
CONCLUSION
Surgical resection of intracranial HPC, in an attempt to reach Simpson grade 1 removal, is necessary for better outcome. Adjuvant RT should be done as recommended before, to prevent recurrence, regardless of surgical resection and pathological diagnosis.
MeSH Terms
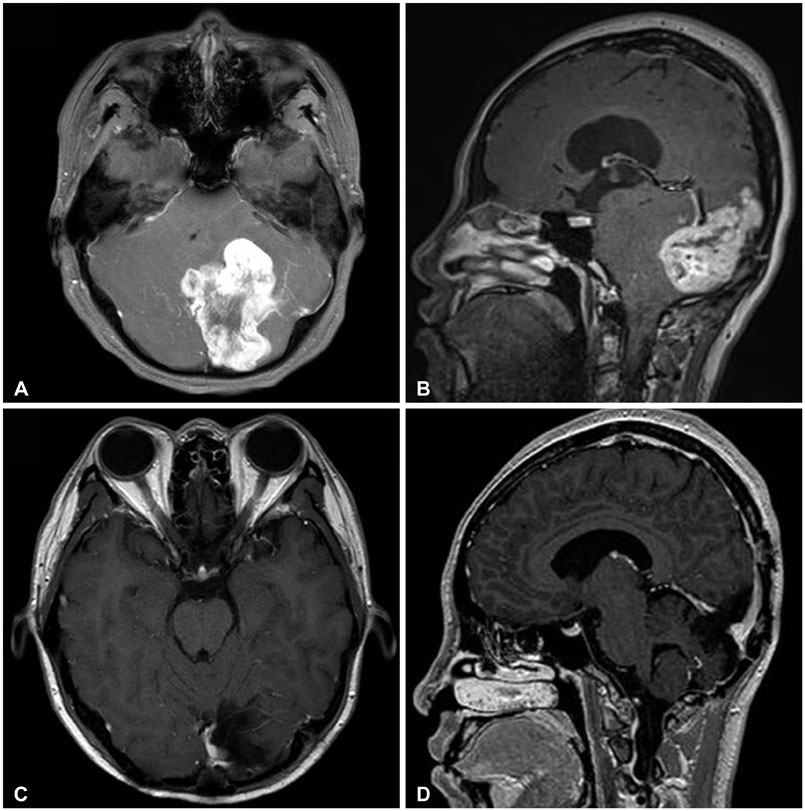
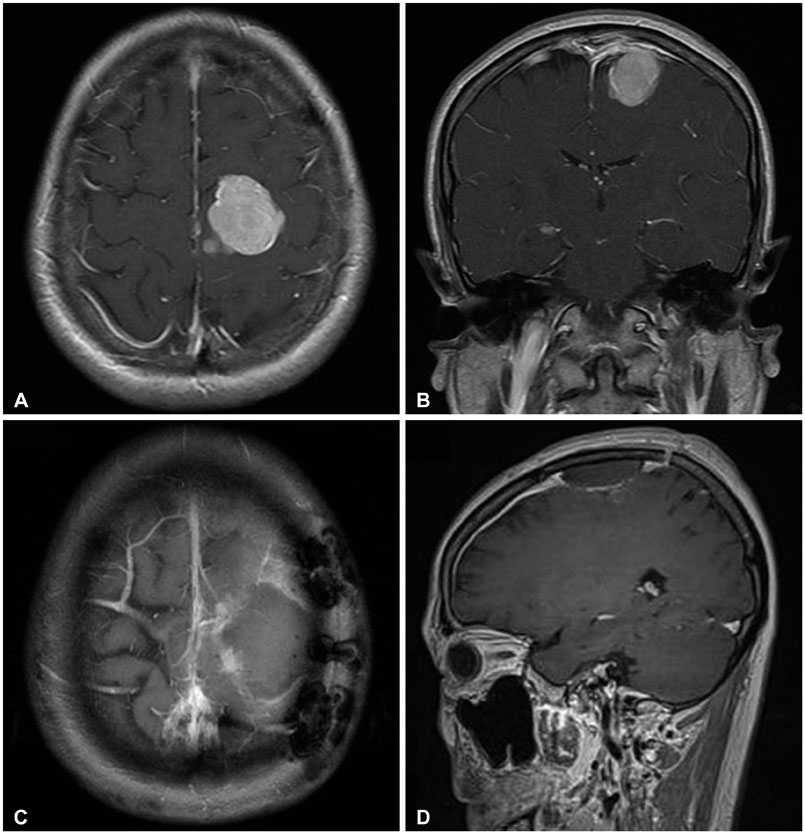
Figure
Reference
-
1. Stout AP, Murray MR. Hemangiopericytoma: a vascular tumor featuring zimmermann's pericytes. Ann Surg. 1942; 116:26–33.
Article2. Dufour H, Métellus P, Fuentes S, et al. Meningeal hemangiopericytoma: a retrospective study of 21 patients with special review of postoperative external radiotherapy. Neurosurgery. 2001; 48:756–762. discussion 762-3
Article3. Goellner JR, Laws ER Jr, Soule EH, Okazaki H. Hemangiopericytoma of the meninges. Mayo Clinic experience. Am J Clin Pathol. 1978; 70:375–380.
Article4. Guthrie BL, Ebersold MJ, Scheithauer BW, Shaw EG. Meningeal hemangiopericytoma: histopathological features, treatment, and long-term follow-up of 44 cases. Neurosurgery. 1989; 25:514–522.
Article5. Park BJ, Kim YI, Hong YK, Jeun SS, Lee KS, Lee YS. Clinical analysis of intracranial hemangiopericytoma. J Korean Neurosurg Soc. 2013; 54:309–316.
Article6. Ghose A, Guha G, Kundu R, Tew J, Chaudhary R. CNS Hemangiopericytoma: A Systematic Review of 523 Patients. Am J Clin Oncol. 2014; 10. 27. [Epub]. DOI: 10.1097/COC.0000000000000146.7. Tian R, Hao S, Hou Z, et al. Clinical characteristics and prognostic analysis of recurrent hemangiopericytoma in the central nervous system: a review of 46 cases. J Neurooncol. 2013; 115:53–59.
Article8. Stessin AM, Sison C, Nieto J, Raifu M, Li B. The role of postoperative radiation therapy in the treatment of meningeal hemangiopericytoma-experience from the SEER database. Int J Radiat Oncol Biol Phys. 2013; 85:784–790.
Article9. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957; 20:22–39.
Article10. Horten BC, Urich H, Rubinstein LJ, Montague SR. The angioblastic meningioma: a reappraisal of the nosological problem. Light-, electron-microscopic, tissue, and organ culture observations. J Neurol Sci. 1977; 31:387–410.11. Rutkowski MJ, Jian BJ, Bloch O, et al. Intracranial hemangiopericytoma: clinical experience and treatment considerations in a modern series of 40 adult patients. Cancer. 2012; 118:1628–1636.12. Kumar N, Kumar R, Kapoor R, et al. Intracranial meningeal hemangiopericytoma: 10 years experience of a tertiary care Institute. Acta Neurochir (Wien). 2012; 154:1647–1651.
Article13. Schiariti M, Goetz P, El-Maghraby H, Tailor J, Kitchen N. Hemangiopericytoma: long-term outcome revisited. Clinical article. J Neurosurg. 2011; 114:747–755.14. Rutkowski MJ, Sughrue ME, Kane AJ, et al. Predictors of mortality following treatment of intracranial hemangiopericytoma. J Neurosurg. 2010; 113:333–339.
Article15. Combs SE, Thilmann C, Debus J, Schulz-Ertner D. Precision radiotherapy for hemangiopericytomas of the central nervous system. Cancer. 2005; 104:2457–2465.
Article16. Kim JH, Jung HW, Kim YS, et al. Meningeal hemangiopericytomas: long-term outcome and biological behavior. Surg Neurol. 2003; 59:47–53. discussion 53-417. Bastin KT, Mehta MP. Meningeal hemangiopericytoma: defining the role for radiation therapy. J Neurooncol. 1992; 14:277–287.
Article18. Bassiouni H, Asgari S, Hübschen U, König HJ, Stolke D. Intracranial hemangiopericytoma: treatment outcomes in a consecutive series. Zentralbl Neurochir. 2007; 68:111–118.
Article19. Fountas KN, Kapsalaki E, Kassam M, et al. Management of intracranial meningeal hemangiopericytomas: outcome and experience. Neurosurg Rev. 2006; 29:145–153.
Article20. Soyuer S, Chang EL, Selek U, McCutcheon IE, Maor MH. Intracranial meningeal hemangiopericytoma: the role of radiotherapy: report of 29 cases and review of the literature. Cancer. 2004; 100:1491–1497.
Article21. Sheehan J, Kondziolka D, Flickinger J, Lunsford LD. Radiosurgery for treatment of recurrent intracranial hemangiopericytomas. Neurosurgery. 2002; 51:905–910. discussion 910-1
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Rare Case of Cerebral Metastasis from Hemangiopericytoma in Pelvis
- Hemangiopericytoma of the Posterior Fossa: A Case Report and Review of the Literature
- Metastasis of Intracranial Hemangiopericytoma to Thoracic Spine
- A case of successfully resected retroperitoneal hemangiopericytoma
- Metastatic Intracranial Hemangiopericytoma to the Spinal Column: A Case Report