J Korean Neurosurg Soc.
2015 Oct;58(4):321-327. 10.3340/jkns.2015.58.4.321.
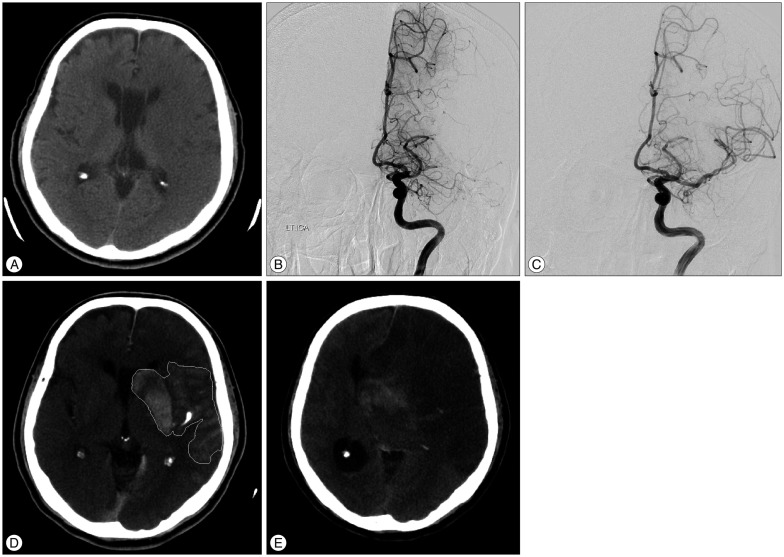
Extent of Contrast Enhancement on Non-Enhanced Computed Tomography after Intra-Arterial Thrombectomy for Acute Infarction on Anterior Circulation: As a Predictive Value for Malignant Brain Edema
- Affiliations
-
- 1Department of Neurosurgery, Cheongju St. Mary's Hospitial, Cheongju, Korea. mrasy@hanmail.net
- KMID: 2114367
- DOI: http://doi.org/10.3340/jkns.2015.58.4.321
Abstract
OBJECTIVE
To determine whether the use of contrast enhancement (especially its extent) predicts malignant brain edema after intra-arterial thrombectomy (IAT) in patients with acute ischemic stroke.
METHODS
We reviewed the records of patients with acute ischemic stroke who underwent IAT for occlusion of the internal carotid artery or the middle cerebral artery between January 2012 and March 2015. To estimate the extent of contrast enhancement (CE), we used the contrast enhancement area ratio (CEAR)-i.e., the ratio of the CE to the area of the hemisphere, as noted on immediate non-enhanced brain computed tomography (NECT) post-IAT. Patients were categorized into two groups based on the CEAR values being either greater than or less than 0.2.
RESULTS
A total of 39 patients were included. Contrast enhancement was found in 26 patients (66.7%). In this subgroup, the CEAR was greater than 0.2 in 7 patients (18%) and less than 0.2 in the other 19 patients (48.7%). On univariate analysis, both CEAR > or =0.2 and the presence of subarachnoid hemorrhage were significantly associated with progression to malignant brain edema (p<0.001 and p=0.004), but on multivariate analysis, only CEAR > or =0.2 showed a statistically significant association (p=0.019). In the group with CEAR > or =0.2, the time to malignant brain edema was shorter (p=0.039) than in the group with CEAR <0.2. Clinical functional outcomes, based on the modified Rankin scale, were also significantly worse in patients with CEAR > or =0.2 (p=0.003)
CONCLUSION
The extent of contrast enhancement as noted on NECT scans obtained immediately after IAT could be predictive of malignant brain edema and a poor clinical outcome.
MeSH Terms
Figure
Reference
-
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20. PMID: 25517348.2. Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke : real-world experience and a call for action. Stroke. 2010; 41:2254–2258. PMID: 20829513.
Article3. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 368:893–903. PMID: 23390923.
Article4. Choi JY, Lee JI, Lee TH, Sung SM, Cho HJ, Ko JK. Emergent recanalization with stenting for acute stroke due to athero-thrombotic occlusion of the cervical internal carotid artery : a single center experience. J Korean Neurosurg Soc. 2014; 55:313–320. PMID: 25237426.
Article5. Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013; 368:904–913. PMID: 23387822.
Article6. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke : a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384:1929–1935. PMID: 25106063.
Article7. Fugate JE, Klunder AM, Kallmes DF. What is meant by "TICI"? AJNR Am J Neuroradiol. 2013; 34:1792–1797. PMID: 23578670.
Article8. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030. PMID: 25671798.
Article9. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137. PMID: 12869717.
Article10. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke : a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947. PMID: 23370205.
Article11. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA. IMS I and II Investigators. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009; 73:1066–1072. PMID: 19786699.
Article12. Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013; 368:914–923. PMID: 23394476.
Article13. Kim H, Jin ST, Kim YW, Kim SR, Park IS, Jo KW. Predictors of malignant brain edema in middle cerebral artery infarction observed on CT angiography. J Clin Neurosci. 2015; 22:554–560. PMID: 25510537.
Article14. Kim JM, Park KY, Lee WJ, Byun JS, Kim JK, Park MS, et al. The cortical contrast accumulation from brain computed tomography after endovascular treatment predicts symptomatic hemorrhage. Eur J Neurol. 2015; 22:1453–1458. PMID: 26130213.
Article15. Kim JT, Heo SH, Cho BH, Choi SM, Lee SH, Park MS, et al. Hyperdensity on non-contrast CT immediately after intra-arterial revascularization. J Neurol. 2012; 259:936–943. PMID: 22015965.
Article16. Lummel N, Schulte-Altedorneburg G, Bernau C, Pfefferkorn T, Patzig M, Janssen H, et al. Hyperattenuated intracerebral lesions after mechanical recanalization in acute stroke. AJNR Am J Neuroradiol. 2014; 35:345–351. PMID: 23907245.
Article17. Nakano S, Iseda T, Kawano H, Yoneyama T, Ikeda T, Wakisaka S. Parenchymal hyperdensity on computed tomography after intra-arterial reperfusion therapy for acute middle cerebral artery occlusion : incidence and clinical significance. Stroke. 2001; 32:2042–2048. PMID: 11546895.
Article18. Pan J, Konstas AA, Bateman B, Ortolano GA, Pile-Spellman J. Reperfusion injury following cerebral ischemia : pathophysiology, MR imaging, and potential therapies. Neuroradiology. 2007; 49:93–102. PMID: 17177065.
Article19. Parrilla G, García-Villalba B, Espinosa de Rueda M, Zamarro J, Carrión E, Hernández-Fernández F, et al. Hemorrhage/contrast staining areas after mechanical intra-arterial thrombectomy in acute ischemic stroke : imaging findings and clinical significance. AJNR Am J Neuroradiol. 2012; 33:1791–1796. PMID: 22538076.
Article20. Wildenhain SL, Jungreis CA, Barr J, Mathis J, Wechsler L, Horton JA. CT after intracranial intraarterial thrombolysis for acute stroke. AJNR Am J Neuroradiol. 1994; 15:487–492. PMID: 8197945.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed tomographic findings of intracranial pyogenic abscess
- Early and Delayed Myocardial Enhancement in Myocardial Infarction Using Two-Phase Contrast-Enhanced Multidetector-Row CT
- Contrast Enhancement Pattern in MR Imaging of Acute Cerebral Infarction
- Predictive Factors for Good Outcome and Mortality After Stent-Retriever Thrombectomy in Patients With Acute Anterior Circulation Stroke
- Primary neurocritical care involving therapeutic hypothermia for acute ischemic stroke patients with malignant infarct cores