J Korean Orthop Assoc.
2012 Jun;47(3):211-215. 10.4055/jkoa.2012.47.3.211.
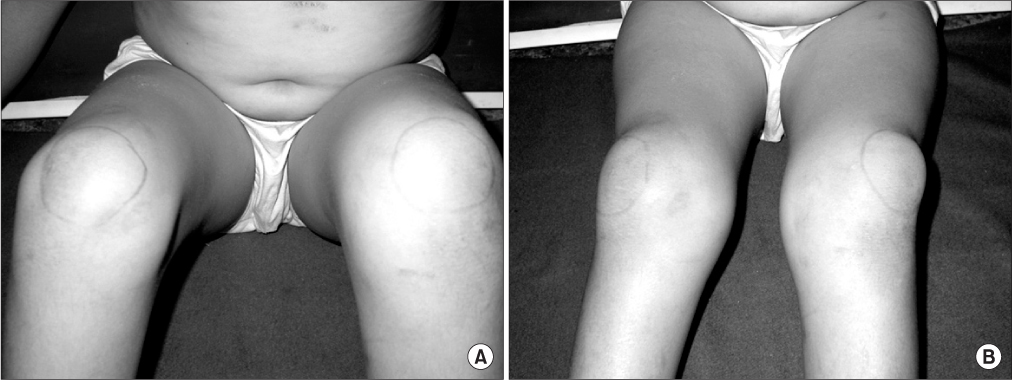
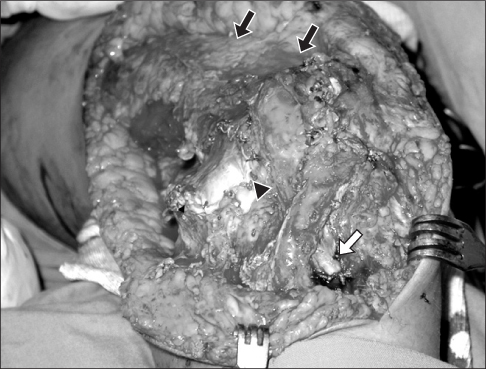
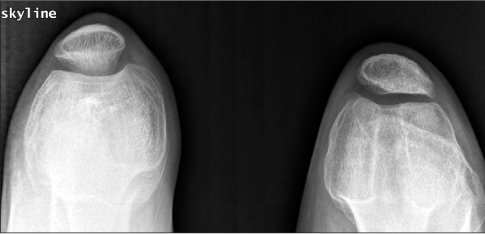
Treatment for Bilateral Congenital Dislocation of the Patella Using Stanisavljevic Procedure
- Affiliations
-
- 1Department of Orthopaedic Surgery, Hanyang University College of Medicine, Seoul, Korea. kimts@hanyang.ac.kr
- KMID: 2106650
- DOI: http://doi.org/10.4055/jkoa.2012.47.3.211
Abstract
- Congenital dislocation of the patella is a rare clinical entity and is considered to result from a failure in internal rotation when the myotome develops, which forms the femur, the quadriceps muscle, and the extensor mechanism. Several authors have suggested various treatment methods, but there has been no consensus on treatment. A 12-year-old boy complained of knee pain and presented with a deformity due to bilateral congenital dislocation of the patella. The patient was treated with surgical management using the Stanisavljevic procedure. We report this case of congenital dislocation of the patella treated with this procedure that achieved a stable patellofemoral joint and satisfactory clinical results over 6.5 years of follow-up. In addition, we have included a review of the relevant medical literature.
MeSH Terms
Figure
Reference
-
1. Ferris B, Aichroth P. The treatment of congenital knee dislocation. A review of nineteen knees. Clin Orthop Relat Res. 1987. 216:135–140.2. Ghanem I, Wattincourt L, Seringe R. Congenital dislocation of the patella. Part I: pathologic anatomy. J Pediatr Orthop. 2000. 20:812–816.
Article3. Bensahel H, Souchet P, Pennecot GF, Mazda K. The unstable patella in children. J Pediatr Orthop B. 2000. 9:265–270.
Article4. Marumo K, Fujii K, Tanaka T, Takeuchi H, Saito H, Koyano Y. Surgical management of congenital permanent dislocation of the patella in nail patella syndrome by Stanisavljevic procedure. J Orthop Sci. 1999. 4:446–449.
Article5. Stanisavljevic S, Zemenick G, Miller D. Congenital, irreducible, permanent lateral dislocation of the patella. Clin Orthop Relat Res. 1976. (116):190–199.
Article6. Eilert RE. Congenital dislocation of the patella. Clin Orthop Relat Res. 2001. 389:22–29.
Article7. Walker J, Rang M, Daneman A. Ultrasonography of the unossified patella in young children. J Pediatr Orthop. 1991. 11:100–102.
Article8. Koplewitz BZ, Babyn PS, Cole WG. Congenital dislocation of the patella. AJR Am J Roentgenol. 2005. 184:1640–1646.
Article9. Chrisman OD, Snook GA, Wilson TC. A long-term prospective study of the Hauser and Roux-Goldthwait procedures for recurrent patellar dislocation. Clin Orthop Relat Res. 1979. (144):27–30.
Article10. Ceynowa M, Mazurek T. Congenital patella dislocation in a child with Rubinstein-Taybi syndrome. J Pediatr Orthop B. 2009. 18:47–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Habitual Patella Dislocation with Genu Valgum
- Irreducible Acute Patellar Dislocation with Anatomical Variant: Notched Patella
- Habitual Dislocation of the Patella: 4 Patients Report
- The Treatment of Bilateral Congenital Dislocation of the Hip
- Treatment of the Patella Using Gracilis as a Static and Dynamic Stabilizer: A Case Report