J Korean Orthop Assoc.
2008 Feb;43(1):57-64. 10.4055/jkoa.2008.43.1.57.
The Total Knee Arthroplasty with PFC Sigma RP-F(R): Two Year Short-term Results
- Affiliations
-
- 1Department of Orthopedic Surgery, Pusan National University Hospital, Busan, Korea. jtsuh@pusan.ac.kr
- KMID: 2106417
- DOI: http://doi.org/10.4055/jkoa.2008.43.1.57
Abstract
-
PURPOSE: This study compared the results of PFC Sigma RP-F(R) total knee arthroplasty with those of conventional total knee arthroplasty using PFC Sigma PS(R) in order to assess the clinical results including the maximal flexion angle after a follow up of at least 2 years.
MATERIALS AND METHODS
Forty one cases of total knee arthroplasty were performed with PFC Sigma RP-F(R), and the clinical results were analyzed after a follow up of at least 2 years. The patients were compared with a control group consisting of 41 cases, who underwent total knee arthroplasty with PFC Sigma PS(R) using the following parameters: gender, preoperative diagnosis, and preoperative range of motion, and postoperative range of motion.
RESULTS
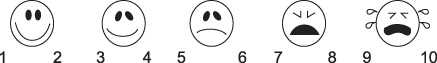
The mean follow up period was 26.7 months. The KSS score improved from 53.2 preoperatively to 95.6 postoperatively. The KSFS score also improved from 49.7 preoperatively to 96.1 postoperatively. The range of motion increased from 124.3degrees to 128.2degrees. The subjective pain score using visual analogue scale improved from 7.6 preoperatively to 1.4 postoperatively. The group with the PFC Sigma RP-F(R) showed similar clinical results to the PFC Sigma PS(R) except for the range of motion.
CONCLUSION
Total knee arthroplasty with PFC Sigma RP-F(R) showed similar clinical results to other models, as well as excellent and predictable results of range of motion at the short-term follow up. A long term follow up study will be needed to demonstrate its effects on increasing the longevity.
Figure
Reference
-
1. Aglietti P, Buzzi R, De Felice R, Giron F. The Insall-Burstein total knee replacement in osteoarthritis: a 10-year minimum follow-up. J Arthroplasty. 1999. 14:560–565.2. Argenson JN, Scuderi GR, Komistek RD, Scott WN, Kelly MA, Aubaniac JM. In vivo kinematic evaluation and design consideration related to high flexion in total knee arthroplasty. J Biomech. 2005. 38:277–284.3. Argenson JN, O'Connor JJ. Polyethylene wear in meniscal knee replacement: A one to nine-year retrieval analysis of the Oxford knee. J Bone Joint Surg Br. 1992. 74:228–232.
Article4. Buechel FF, Pappas MJ. The New Jersey low-contact-stress knee replacement system : biomechanical rationale and review of the first 123 cemented cases. Arch Orthop Trauma Surg. 1986. 105:197–204.5. Callaghan JJ, Squire MW, Goetz DD, Sullivan PM, Johnston RC. Cemented ratating-platform total knee replacement: a nine to twelve-year follow-up study. J Bone Joint Surg Am. 2000. 82:705–711.6. Dennis DA, Komistek RD, Colwell CE Jr, et al. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Ciln Orthop Relat Res. 1998. 356:47–57.7. D'Lima DD, Trice M, Urguhart AG, Colwell CW Jr. Tibiofemoral conformity and kinematics of rotating-bearing knee prosthesis. Clin Orthop Relat Res. 2001. 386:235–242.8. Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ. Measuring flexion in knee arthroplasty patients. J Arthoplasty. 2004. 19:369–372.
Article9. Goodfellow JW, O'Connor J. Clinical results of the Oxford knee: Surface arthroplasty of the tibiofemoral joint with meniscal bearing prosthesis. Clin Orthop Relat Res. 1986. 205:21–42.10. Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA. Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br. 1993. 75:950–955.
Article11. Huang CH, Ma HM, Liau JJ, Ho FY, Cheng CK. Late dislocation of rotating platform in New Jersey low-contact stress knee prosthesis. Clin Orthop Realt Res. 2002. 405:189–194.
Article12. Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty. A minimum of 2 years of follow-up. J Arthroplasty. 2005. 20:674–679.
Article13. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989. 248:13–14.
Article14. Jung YB, Kim JS, Tae SK, Jung HJ, Kim JW. Medium term results of a mobile bearing total knee replacement. J Korean Orthop Assoc. 2003. 38:678–682.
Article15. Kim YH, Kook HK, Kim JS. Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res. 2001. 392:101–115.
Article16. Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972. 52:34–43.
Article17. Maloney WJ, Schurman DJ. The effect of implant design on range of motion after total knee arthroplasty. Total condylar versus posterior stabilized total condylar designs. Clin Orthop Relat Res. 1992. 278:147–152.18. McAuley JP, Harrer MF, Ammeen D, Engh GA. Outcome of knee arthroplasty in patient with poor preoperative range of motion. Clin Orthop Relat Res. 2002. 404:203–207.19. Mcewen HM, Fisher J, Goldsmith AA, Auger DD, Hardaker C, Stone MH. Wear of fixed bearing and rotating platform mobile bearing knees subjected to high levels of internal and external tibial rotation. J Mater Sci Mater Med. 2001. 12:1049–1052.20. Mulholland SJ, Wyss UP. Activities of daily living on non-Western culture: range of motion requirements for hip and knee joint implantation. Int J Rehabil Res. 2001. 24:191–198.21. Myles CM, Rowe PJ, Walker CR, Nutton RW. Knee joint functional range of motion prior to and following total knee arthroplsty measured using flexible electrogoniometry. Gait Posture. 2002. 16:46–54.22. Otto JK, Callaghan JJ, Brown TD. Gait cycle finite element comparison of ratating-platform total knee disigns. Clin Orthop Relat Res. 2003. 410:181–188.23. Price AJ, Rees JL, Beard D. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicenter single-blind randomised controlled trial. J Bone Joint Surg Br. 2003. 85:62–67.24. Ranawat AS, Rossi R, Loreti I, Rasquinha VJ, Rodriguez JA, Ranawat CS. Comparison of the PFC sigma fixed-bearing and rotating-platform total knee arthroplasty in the same patient: short term results. J Arthroplasty. 2004. 19:35–39.25. Rowe PJ, Myles CM, Walker C, Nutton R. Knee joint kinematics in flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture. 2000. 12:143–155.26. Schurman DJ, Parker JN, Ornstein D. Total condylar knee replacement. J Bone Joint Surg Am. 1985. 67:1006–1014.27. Seon JK, Song EK, Lee JY. Comparison of range of motion of high-flexion prosthesis and mobile bearing prosthesis in total knee arthroplasty. Orthopedics. 2005. 28:Suppl 10. 1247–1250.
Article28. Shin JY, Kho DH, Kim DH, Jung JK. The short-term results of PFC Sigma Rotating-Platform in total knee arthroplasty. J Korean Knee Soc. 2004. 16:15–20.29. Walker PS, Garg A. Range of motion in total knee arthroplasty. A computer analysis. Clin Orthop Relat Res. 1991. 262:227–235.30. Woolson ST, Northrop GD. Mobile- vs. fixed-bearing total knee arthroplasty. A clinical and radiologic study. J Arthroplasty. 2004. 19:135–140.31. Yamakado K, Kitaoka K, Yamada H, Hashiba K, Nakamura R, Tomita K. Influence of stability on range of motion after cruciate-retaining TKA. Arch Orthop Trauma Surg. 2003. 123:1–4.
Article32. Yamazaki J, Ishigami S, Nagashima M, Yoshino S. Hy-Flex II tatal knee system and range of motion. Arch Orthop Trauma Surg. 2002. 122:156–160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mid-term Results of Total Knee Arthroplasty Using PFC Sigma RP-F
- The Short-term Results of PFC Sigma Rotating-Platform in Total Knee Arthroplasty
- Comparison of the Clinical Outcomes after Total Knee Arthroplasty with the LCS Rotating Platform Mobile Bearing Knee System and the PFC Sigma RP-F Mobile Bearing Knee System
- A Comparison of the Clinical and Radiographic Results of Press Fit Condylar Rotating-Platform High-Flexion and Low Contact Stress Mobile Bearing Prosthesis in Total Knee Arthroplasty: Short term Results
- Moderate to Severe Varus Deformity in Total Knee Arthroplasty: PFC Sigma Fixed Bearing Versus Rotating Platform