J Korean Orthop Assoc.
2007 Feb;42(1):106-114. 10.4055/jkoa.2007.42.1.106.
Agonistforthe Control of Apotosis through the Study of Cytokine Expression after Spinal CordInjuryin Rats
- Affiliations
-
- 1Department of Orthopaedic Surgery, School of Medicine, Chungnam National University, Research Institute of Medical Sciences, Daejeon, Korea. jyyang@cnuh.co.kr
- 2Barnes-Jewish Hospital, Washington University, USA.
- KMID: 2106383
- DOI: http://doi.org/10.4055/jkoa.2007.42.1.106
Abstract
-
Purpose: To analyze the cytokines that appear after a spinal cord injury in rats and to determine the agonists that regulate apoptosis.
Materials and Methods
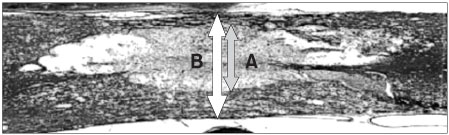
Sixty female Sprague-Dawley rats were anesthetized, and a laminectomy was performed at the 9th thoracic vertebra. The spinal cord injury was induced by dropping a 10 gm weight at a height of 20 mm. The subjects were divided into 5 groups. Group I was administered aminoguanidine, group II was administered GM-CSF, group III was administered riluzole, group IV was administered erythropoietin, and group V was administered methylprednisolone. A control group was administered normal saline. The results were assessed using the Tarlov motor grading method. In 1, 3, 5 and 7 days after the spinal cord injury, the rats were sacrificed and evaluated using the syringomyelic cavity size. Immunohistochemical staining for e-NOS and RT-PCR for XIAP were also performed.
Results
Groups I, III, and V showed significantly different results in terms of the motor recovery and inhibition of increase in the syringomyelic cavity compared with the other groups (p<0.05). The e-NOS activity was observed in groups I, III, and V. The other groups showed almost no e-NOS activity. On the RT-PCR, groups I, III, and V showed significantly different results in terms of XIAP expression with time compared with the other groups.
Conclusion
Steroids, NOS inhibitors and sodium channel inhibitors appear to be important factors for regulating apoptosis in the early stage of a spinal cord injury. Further study will be needed to develop new pharmaceuticals with synergic effects on spinal cord injuries.
Keyword
MeSH Terms
-
Animals
Apoptosis
Cytokines
Erythropoietin
Female
Granulocyte-Macrophage Colony-Stimulating Factor
Humans
Laminectomy
Methylprednisolone
Rats*
Rats, Sprague-Dawley
Riluzole
Sodium Channel Blockers
Spinal Cord Injuries
Spine
Steroids
Cytokines
Erythropoietin
Granulocyte-Macrophage Colony-Stimulating Factor
Methylprednisolone
Riluzole
Sodium Channel Blockers
Steroids
Figure
Reference
-
1. Bracken MB. Methylprednisolone and acute spinal cord injury: an update of the randomized evidence. Spine. 2001. 26:24 Suppl. S55.2. Bracken MB, Shepard MJ, Holford TR, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA. 1997. 277:1597–1604.
Article3. Braughler JM, Hall ED. Correlation of methylprednisolone levels in cat spinal cord with its effects on (Na++K+)-ATPase, lipid peroxidation, and alpha motor neuron function. J Neurosurg. 1982. 56:838–844.4. Braughler JM, Hall ED, Means ED, Waters TR, Anderson DK. Evaluation of an intensive methylprednisolone sodium succinate dosing regimen in experimental spinal cord injury. J Neurosurg. 1987. 67:102–105.
Article5. Brines M. What evidence supports use of erythropoietin as a novel neurotherapeutic? Oncology (Williston Park). 2002. 16:9 Suppl 10. S79–S89.6. Doble A. The pharmacology and mechanism of action of riluzole. Neurology. 1996. 47:6 Suppl 4. S233–S241.
Article7. Faden AI, Demediuk P, Panter SS, Vink R. The role of excitatory amino acids and NMDA receptors in traumatic brain injury. Science. 1989. 244:798–800.
Article8. Ha Y, Kim YS, Cho JM, et al. Role of granulocyte-macrophage colony-stimulating factor in preventing apoptosis and improving functional outcome in experimental spinal cord contusion injury. J Neurosurg Spine. 2005. 2:55–61.
Article9. Huang CS, Song JH, Nagata K, Yeh JZ, Narahashi T. Effects of the neuroprotective agent riluzole on the high voltage-activated calcium channels of rat dorsal root ganglion neurons. J Pharmacol Exp Ther. 1997. 282:1280–1290.10. Kannan Y, Moriyama M, Sugano T, et al. Neurotrophic action of interleukin 3 and granulocyte-macrophage colony-stimulating factor on murine sympathetic neurons. Neuroimmunomodulation. 2000. 8:132–141.
Article11. Mu X, Azbill RD, Springer JE. Riluzole improves measures of oxidative stress following traumatic spinal cord injury. Brain Res. 2000. 870:66–72.
Article12. Sekhon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine. 2001. 26:24 Suppl. S2–S12.
Article13. Sekiguchi Y, Kikuchi S, Myers RR, Campana WM. ISSLS prize winner: Erythropoietin inhibits spinal neuronal apoptosis and pain following nerve root crush. Spine. 2003. 28:2577–2584.
Article14. Song JH, Huang CS, Nagata K, Yeh JZ, Narahashi T. Differential action of riluzole on tetrodotoxin-sensitive and tetrodotoxin-resistant sodium channels. J Pharmacol Exp Ther. 1997. 282:707–714.15. Soy O, Aslan O, Uzun H, et al. Time-level relationship for nitric oxide and the protective effects of aminoguanidine in experimental spinal cord injury. Acta Neurochir (Wien). 2004. 146:1329–1335.
Article16. Tarlov IM. Acute spinal cord compression paralysis. J Neurosurg. 1972. 36:10–20.
Article17. Tator CH. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol. 1995. 5:407–413.
Article18. Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg. 1991. 75:15–26.
Article19. Young W, Flamm ES. Effect of high-dose corticosteroid therapy on blood flow, evoked potentials, and extracellular calcium in experimental spinal injury. J Neurosurg. 1982. 57:667–673.
Article20. Wada K, Chatzipanteli K, Kraydieh S, Busto R, Dietrich WD. Inducible nitric oxide synthase expression after traumatic brain injury and neuroprotection with aminoguanidine treatment in rats. Neurosurgery. 1998. 43:1427–1436.
Article21. Zhang F, Iadecola C. Temporal characteristics of the protective effect of aminoguanidine on cerebral ischemic damage. Brain Res. 1998. 802:104–110.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Changes of Neurologic Injury and Cytokine mRNA Expression according to Spinal Ischemia Time in the Rat
- Increased expression of osteopontin in the spinal cords of Lewis rats with experimental autoimmune neuritis
- Fos Expression in the Brain of Neuropathic Pain Rats
- Study on the nNOS Expression in the Rat Spinal Cord of the Spinal Nerve Ligation Model with Neuropathic Pain and the Dorsal Rhizotomy
- Effects of Electrical Stimulation and Weight-Supported Treadmill Gait Simulation on Apoptosis in the Muscles of Rats with Spinal Cord Injury