J Korean Surg Soc.
2011 Nov;81(5):344-349. 10.4174/jkss.2011.81.5.344.
Hungry bone syndrome after parathyroidectomy of a minimally invasive parathyroid carcinoma
- Affiliations
-
- 1Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea. mdkang@yonsei.ac.kr
- KMID: 2096689
- DOI: http://doi.org/10.4174/jkss.2011.81.5.344
Abstract
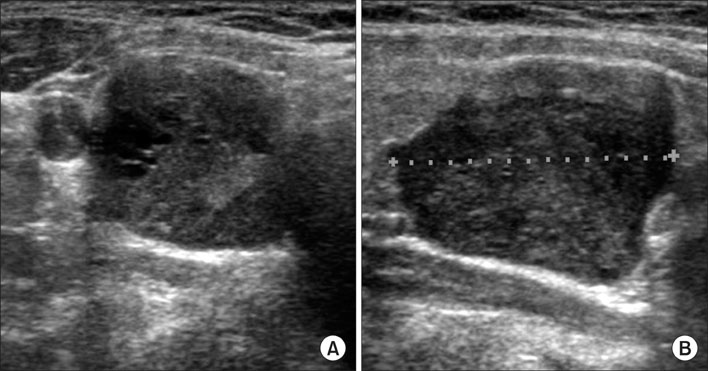
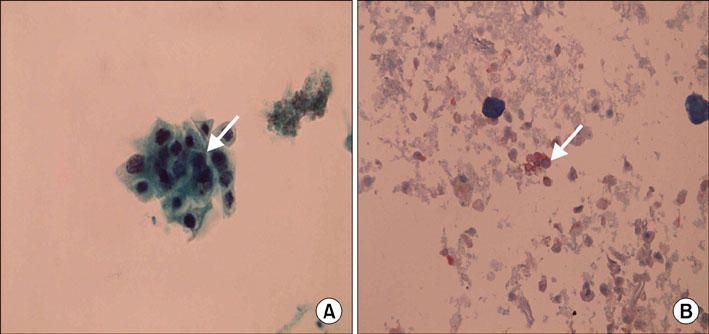
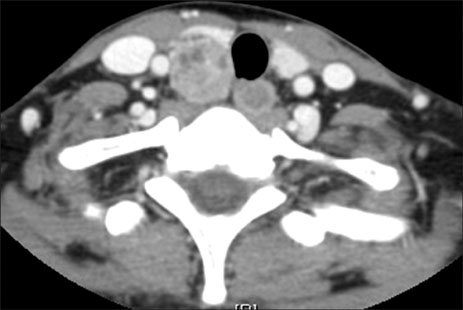
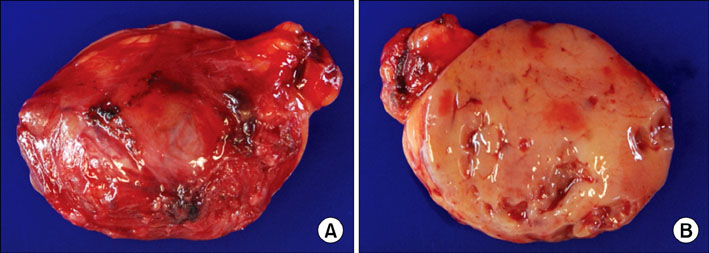
- The prognosis of parathyroid carcinoma varies significantly between numerous studies. Therefore, many attempts have been made to grade the degree of parathyroid carcinoma, and recently, classifying parathyroid carcinomas into either minimally invasive or widely invasive carcinoma- similar to follicular carcinoma of the thyroid- has led to a more reliable prediction of the prognosis. Hungry bone syndrome can occur if parathyroidectomy is performed due to primary hyperparathyroidism regardless of the cause of the disease. Hungry bone syndrome is characterized by postoperative a hypocalcemic state due to remineralization of various minerals, including calcium, of the bone; this syndrome requires a long-term supplementation of calcium. The authors aim to report, along with a review of related literatures, 1 case of a 29-year-old female patient diagnosed with minimally invasive parathyroid carcinoma who fell into hungry bone syndrome after parathyroidectomy.
MeSH Terms
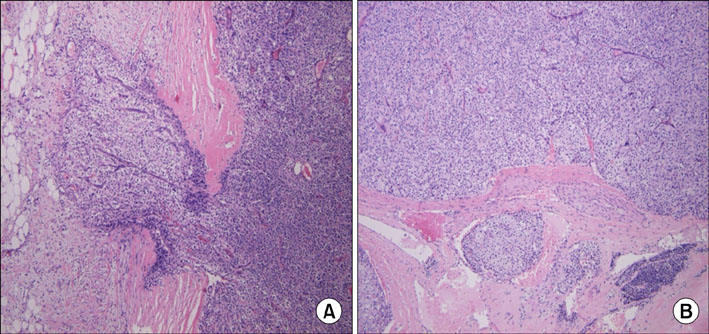
Figure
Reference
-
1. Melton LJ 3rd. The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res. 2002. 17:Suppl 2. N12–N17.2. Wynne AG, van Heerden J, Carney JA, Fitzpatrick LA. Parathyroid carcinoma: clinical and pathologic features in 43 patients. Medicine (Baltimore). 1992. 71:197–205.3. Chang HS, Yoon JH, Chung WY, Park CS. Coexistence of parathyroid and papillary thyroid carcinoma. J Korean Surg Soc. 2004. 66:147–152.4. Kini U, Shariff S, Thomas JA. Ultrasonically guided fine needle aspiration of the parathyroid. A report of two cases. Acta Cytol. 1993. 37:747–751.5. Tseng FY, Hsiao YL, Chang TC. Ultrasound-guided fine needle aspiration cytology of parathyroid lesions. A review of 72 cases. Acta Cytol. 2002. 46:1029–1036.6. Bondeson L, Bondeson AG, Nissborg A, Thompson NW. Cytopathological variables in parathyroid lesions: a study based on 1,600 cases of hyperparathyroidism. Diagn Cytopathol. 1997. 16:476–482.7. Shane E, Bilezikian JP. Parathyroid carcinoma: a review of 62 patients. Endocr Rev. 1982. 3:218–226.8. Shane E. Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab. 2001. 86:485–493.9. Bondeson L, Sandelin K, Grimelius L. Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol. 1993. 17:820–829.10. Kameyama K, Takami H. Proposal for the histological classification of parathyroid carcinoma. Endocr Pathol. 2005. 16:49–52.11. Brasier AR, Nussbaum SR. Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med. 1988. 84:654–660.12. Liu F, Gnepp DR, Pisharodi LR. Fine needle aspiration of parathyroid lesions. Acta Cytol. 2004. 48:133–136.13. Lerud KS, Tabbara SO, DelVecchio DM, Frost AR. Cytomorphology of cystic parathyroid lesions: report of four cases evaluated preoperatively by fine-needle aspiration. Diagn Cytopathol. 1996. 15:306–311.14. Boeckler P, Grunenberger F, Ruellan A, Vignon F, Weber JC, Bachellier P, et al. Hungry bone syndrome after surgical treatment of severe primary hyperparathyroidism: about 3 cases. Ann Endocrinol (Paris). 2002. 63:8–12.15. Albright F, Reifenstein EC. The parathyroid glands and metabolic bone disease. 1948. Balltimore: William & Wilkins.16. Mizrachi A, Gilat H, Bachar G, Feinmesser R, Shpitzer T. Elevated parathyroid hormone levels after parathyroidectomy for primary hyperparathyroidism. Head Neck. 2009. 31:1456–1460.17. Mittendorf EA, McHenry CR. Persistent parathyroid hormone elevation following curative parathyroidectomy for primary hyperparathyroidism. Arch Otolaryngol Head Neck Surg. 2002. 128:275–279.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Hungry Bone Syndrome after Huge Parathyroidectomy
- A Case of Hungry Bone Syndrome after Removal of a Parathyroid Adenoma
- Impact of enhanced recovery after surgery program for hungry bone syndrome in patients on maintenance hemodialysis undergoing parathyroidectomy for secondary hyperparathyroidism
- Bilateral tension pneumothoraces during minimally invasive parathyroidectomy: A case report
- A Case of Hungry Bone Syndrome after Parathyroidectomy in Patient with Tertiary Hyperparathyroidism and Hemodialysis Patient