Korean Circ J.
2011 Sep;41(9):512-517. 10.4070/kcj.2011.41.9.512.
The Primary Patency of Percutaneous Transluminal Angioplasty in Hemodialysis Patients With Vascular Access Failure
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Mokdong Hospital, School of Medicine, Ewha Womans University, Seoul, Korea.
- 2Department of Radiology, Mokdong Hospital, School of Medicine, Ewha Womans University, Seoul, Korea. kangbc@ewha.ac.kr
- KMID: 2094103
- DOI: http://doi.org/10.4070/kcj.2011.41.9.512
Abstract
- BACKGROUND AND OBJECTIVES
Dysfunction of arteriovenous fistulas (AVFs) and arteriovenous grafts (AVGs) contributes significantly to morbidity and hospitalization in the dialysis population. We evaluated the primary patency of AVFs following percutaneous transluminal angioplasty (PTA) in haemodialysis patients.
SUBJECTS AND METHODS
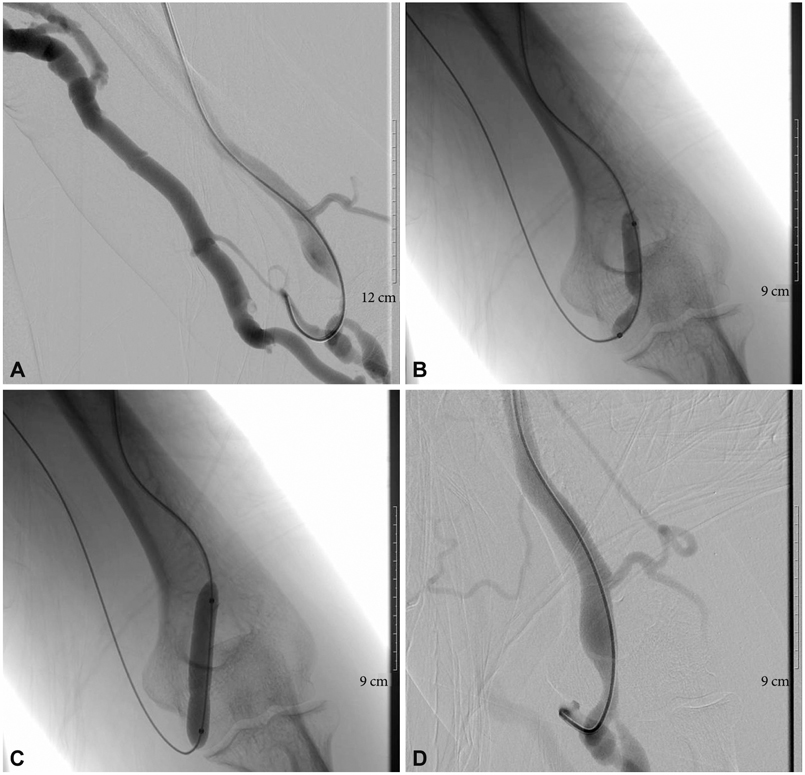
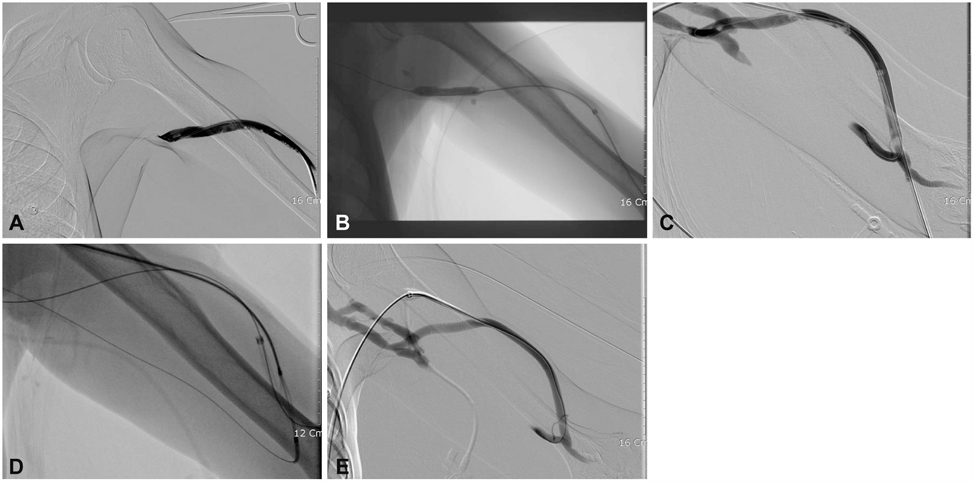
We performed 231 interventions in 118 patients with a mean age of 62.1+/-12.9 years. We performed 122 interventions in 53 AVG patients (44.9%), and 109 interventions in 65 AVF patients (55.1%). If there was thrombosis of the vascular access, urokinase was administered and/or thrombus aspiration was performed. The stent was inserted when balloon dilatation did not expand sufficiently or elastic recoil occurred.
RESULTS
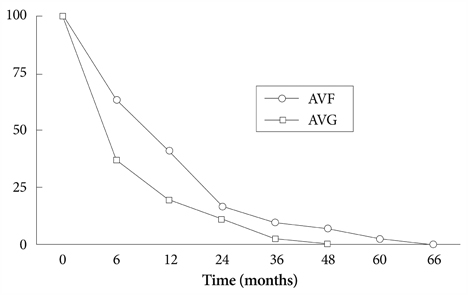
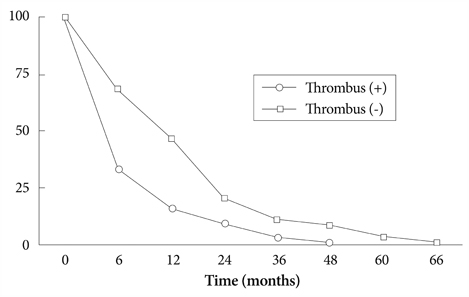
For the 118 patients, the median patency time was 10.45+/-10.29 months at 92 months of follow-up. The primary patencies for stenotic AVFs at 6, 12, 24, 36, 48, and 60 months were 63.4%, 41.4%, 17.0%, 9.7%, 7.3%, and 2.4%, respectively. The primary patencies for AVGs at 6, 12, 24, and 36 months were 36.9%, 19.5%, 10.8%, 2.1%, respectively, and were obtained by means of the Kaplan-Meier analysis (log rank=6.42, p<0.05). The median patency time was 11.0 months and 4.45 months in the non-thrombus and thrombus groups, respectively. The complication rate was 1.73% (4/231); two cases of pseudoaneurysms and two cases of extravasation were detected. All therapy failures (5/231) occurred in thrombotic lesions of AVGs and were treated surgically.
CONCLUSION
PTA is an efficacious method for the correction of stenosis of AVFs for hemodialysis, thus prolonging the patency of the fistulas.
MeSH Terms
Figure
Reference
-
1. Surlan M, Popovic P. The role of interventional radiology in management of patients with end-stage renal disease. Eur J Radiol. 2003. 46:96–114.2. Haage P, Gunther RW. Radiological intervention to maintain vascular access. Eur J Vasc Endovasc Surg. 2006. 32:84–89.3. Dougherty MJ, Calligaro KD, Schindler N, Raviola CA, Ntoso A. Endovascular versus surgical treatment for thrombosed hemodialysis grafts: a prospective, randomized study. J Vasc Surg. 1999. 30:1016–1023.4. Guerra A, Raynaud A, Beyssen B, Pagny JY, Sapoval M, Angel C. Arterial percutaneous angioplasty in upper limbs with vascular access devices for haemodialysis. Nephrol Dial Transplant. 2002. 17:843–851.5. Tang S, Lo CY, Tso WK, Li FK, Chan TM. Percutaneous transluminal angioplasty for stenosis of arteriovenous fistulae: a review of local experience. Hong Kong Med J. 1998. 4:36–41.6. Coskun M, Boyvat F, Kurt A, Agildere AM, Niron EA, Bilgin N. Percutaneous balloon angioplasty for permanent hemodialysis with direct arteriovenous fistulae. Transplant Proc. 1998. 30:816–818.7. Miquelin DG, Reis LF, da Silva AA, de Godoy JM. Percutaneous transluminal angioplasty in the treatment of stenosis of arteriovenous fistulae for hemodialysis. Int Arch Med. 2008. 1:16.8. Lahoche A, Beregi JP, Kherbek K, Willoteaux S, Desmoucelle F, Foulard M. Percutaneous angioplasty of arteriovenous (Brescia-Cimino) fistulae in children. Pediatr Nephrol. 1997. 11:468–472.9. Probst P, Mahler F, Krneta A, Descoeudres C. Percutaneous transluminal dilatation for restoration of angioaccess in chronic hemodialysis patients. Cardiovasc Intervent Radiol. 1982. 5:257–259.10. Campos RP, Do Nascimento MM, Chula DC, Do Nascimento DE, Riella MC. Stenosis in hemodialysis arteriovenous fistula: evaluation and treatment. Hemodial Int. 2006. 10:152–161.11. Roy-Chaudhury P, Kelly BS, Miller MA, et al. Venous neointimal hyperplasia in polytetrafluoroethylene dialysis grafts. Kidney Int. 2001. 59:2325–2334.12. Oakes D, Sherck J, Cobb L. Surgical salvage of failed radiocephalic ateriovenous fistulae: techniques and results in 29 patients. Kidney Int. 1998. 53:480–487.13. Hodges TC, Fillinger MF, Zwolak RM, Walsh DB, Bech F, Cronenwett JL. Longitudinal comparison of dialysis access methods: risk factors for failure. J Vasc Surg. 1997. 26:1009–1019.14. Vorwerk D, Schurmann K, Muller-Leisse C, et al. Hydrodynamic thrombectomy of haemodialysis grafts and fistulae: results of 51 procedures. Nephrol Dial Transplant. 1996. 11:1058–1064.15. Overbosch EH, Pattynama PM, Aarts HJ, Schultze Kook LJ, Hermans J, Reekers JA. Occluded hemodialysis shunts: Dutch multicenter experience with the hydrolyser catheter. Radiology. 1996. 201:485–488.16. Turmel-Rodrigues L, Sapoval M, Pengloan J, et al. Manual thromboaspiration and dilation of thrombosed dialysis access: mid-term results of a simple concept. J Vasc Interv Radiol. 1997. 8:813–824.17. Turmel-Rodrigues L, Pengloan J, Rodrigue H, et al. Treatment of failed native arteriovenous fistulae for hemodialysis by interventional radiology. Kidney Int. 2000. 57:1124–1140.18. Manninen HI, Kaukanen ET, Ikaheimo R, et al. Brachial arterial access: endovascular treatment of failing Brescia-Cimino hemodialysis fistulas: initial success and long-term results. Radiology. 2001. 218:711–718.19. Kim JH, Do YS, Shin SW, et al. Percutaneous intervention for permanent hemodialysis access. J Korean Radiol Soc. 2003. 48:29–37.20. Landwehr P, Lackner K, Gotz R. Dilatation and balloon-expandable stents for the treatment of central venous stenosis in dialysis patients. Rofo. 1990. 153:239–245.21. Oderich GS, Treiman GS, Schneider P, Bhirangi K. Stent placement for treatment of central and peripheral venous obstruction: a long-term multi-institutional experience. J Vasc Surg. 2000. 32:760–769.22. Haage P, Vorwerk D, Piroth W, Schuermann K, Guenther RW. Treatment of hemodialysis-related central venous stenosis or occlusion: results of primary Wallstent placement and follow-up in 50 patients. Radiology. 1999. 212:175–180.23. Verstandig AG, Bloom AI, Sasson T, Haviv YS, Rubinger D. Shortening and migration of Wallstents after stenting of central venous stenoses in hemodialysis patients. Cardiovasc Intervent Radiol. 2003. 26:58–64.24. Pruitt A, Dodson TF, Najibi S, et al. Distal septic emboli and fatal brachiocephalic artery mycotic pseudoaneurysm as a complication of stenting. J Vasc Surg. 2002. 36:625–628.25. Sands JJ, Patel S, Plaviak DJ, Miranda CL. Pharmacomechanical thrombolysis with urokinase for treatment of thrombosed hemodialysis access grafts. ASAIO J. 1994. 40:M886–M888.26. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992. 42:1390–1397.27. Schwab SJ, Raymond JR, Saeed M, Newman GE, Dennis PA, Bollinger RR. Prevention of hemodialysis fistula thrombosis. Early detection of venous stenoses. Kidney Int. 1989. 36:707–711.28. Haage P, Vorwerk D, Wildberger JE, Piroth W, Schürmann K, Günther RW. Percutaneous treatment of thrombosed primary arteriovenous hemodialysis access fistulae. Kidney Int. 2000. 57:1169–1175.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vascular Interventional Procedures Often Encountered by Primary Physicians
- Endovascular Therapy to Salvage Hemodialysis Access
- Early Dysfunction of Radiocephalic Arteriovenous Fistula: Primary and Secondary Patency Rate of Percutaneous Angioplasty
- Percutaneous Transluminal Angioplasty and Thrombolysis in the Management of Insufficient Hemodialysis Access: Long-Term Patency Rates and Factors Affecting Patency Rates
- Clinical outcome of percutaneous thrombectomy of dialysis access thrombosis by an interventional nephrologist