Korean J Pain.
2014 Apr;27(2):139-144. 10.3344/kjp.2014.27.2.139.
Epidural Infusion of Morphine and Levobupivacaine through a Subcutaneous Port for Cancer Pain Management
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea. kimwm@chonnam.ac.kr
- KMID: 2074060
- DOI: http://doi.org/10.3344/kjp.2014.27.2.139
Abstract
- BACKGROUND
To manage intractable cancer pain, an alternative to systemic analgesics is neuraxial analgesia. In long-term treatment, intrathecal administration could provide a more satisfactory pain relief with lower doses of analgesics and fewer side-effects than that of epidural administration. However, implantable drug delivery systems using intrathecal pumps in Korea are very expensive. Considering cost-effectiveness, we performed epidural analgesia as an alternative to intrathecal analgesia.
METHODS
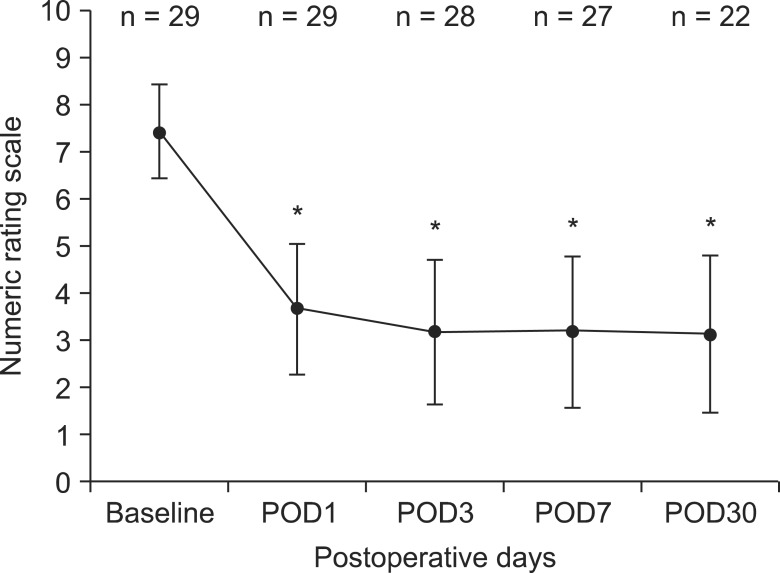
We retrospectively investigated the efficacy, side effects, and complications of epidural morphine and local anesthetic administration through epidural catheters connected to a subcutaneous injection port in 29 Korean terminal cancer patients. Patient demographic data, the duration of epidural administration, preoperative numerical pain rating scales (NRS), side effects and complications related to the epidural catheterization and the drugs, and the numerical pain rating scales on the 1st, 3rd, 7th and 30th postoperative days were determined from the medical records.
RESULTS
The average score for the numerical pain rating scales for the 29 patients decreased from 7 +/- 1.0 at baseline to 3.6 +/- 1.4 on postoperative day 1 (P < 0.001). A similar decrease in pain intensity was maintained for 30 days (P < 0.001). Nausea and vomiting were the most frequently reported side effects of the epidural analgesia and two patients (6.9%) experienced paresthesia.
CONCLUSIONS
Epidural morphine and local anesthetic infusion with a subcutaneous pump seems to have an acceptable risk-benefit ratio and allows a high degree of autonomy to patients with cancer pain.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Anatomic Variations of Cervical and High Thoracic Ligamentum Flavum
Sang Pil Yoon, Hyun Jung Kim, Yun Suk Choi
Korean J Pain. 2014;27(4):321-325. doi: 10.3344/kjp.2014.27.4.321.
Reference
-
1. Nordberg G. Epidural versus intrathecal route of opioid administration. Int Anesthesiol Clin. 1986; 24:93–111. PMID: 2872171.
Article2. Morgan M. The rational use of intrathecal and extradural opioids. Br J Anaesth. 1989; 63:165–188. PMID: 2669907.
Article3. Nitescu P, Appelgren L, Linder LE, Sjöberg M, Hultman E, Curelaru I. Epidural versus intrathecal morphine-bupivacaine: assessment of consecutive treatments in advanced cancer pain. J Pain Symptom Manage. 1990; 5:18–26. PMID: 2324557.
Article4. Crul BJ, Delhaas EM. Technical complications during long-term subarachnoid or epidural administration of morphine in terminally ill cancer patients: a review of 140 cases. Reg Anesth. 1991; 16:209–213. PMID: 1911496.5. Kim JH, Jung JY, Cho MS. Continuous intrathecal morphine administration for cancer pain management using an intrathecal catheter connected to a subcutaneous injection port: a retrospective analysis of 22 terminal cancer patients in Korean population. Korean J Pain. 2013; 26:32–38. PMID: 23342205.
Article7. Krames ES. Intraspinal opioid therapy for chronic nonmalignant pain: current practice and clinical guidelines. J Pain Symptom Manage. 1996; 11:333–352. PMID: 8935137.
Article8. Nitescu P, Sjöberg M, Appelgren L, Curelaru I. Complications of intrathecal opioids and bupivacaine in the treatment of "refractory" cancer pain. Clin J Pain. 1995; 11:45–62. PMID: 7540439.
Article10. Ross VH, Pan PH, Owen MD, Seid MH, Harris L, Clyne B, et al. Neostigmine decreases bupivacaine use by patient-controlled epidural analgesia during labor: a randomized controlled study. Anesth Analg. 2009; 109:524–531. PMID: 19377050.
Article11. Du Pen SL, Peterson DG, Williams A, Bogosian AJ. Infection during chronic epidural catheterization: diagnosis and treatment. Anesthesiology. 1990; 73:905–909. PMID: 2240680.12. Smitt PS, Tsafka A, Teng-van de, van der Holt R, Elswijk-de Vries I, Elfrink E, et al. Outcome and complications of epidural analgesia in patients with chronic cancer pain. Cancer. 1998; 83:2015–2022. PMID: 9806662.
Article13. Maki DG, Ringer M, Alvarado CJ. Prospective randomised trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. Lancet. 1991; 338:339–343. PMID: 1677698.
Article14. De Cicco M, Matovic M, Castellani GT, Basaglia G, Santini G, Del Pup C, et al. Time-dependent efficacy of bacterial filters and infection risk in long-term epidural catheterization. Anesthesiology. 1995; 82:765–771. PMID: 7533485.
Article15. Waghorn DJ. Intravascular device-associated systemic infections: a 2 year analysis of cases in a district general hospital. J Hosp Infect. 1994; 28:91–101. PMID: 7844353.
Article16. de Jong PC, Kansen PJ. A comparison of epidural catheters with or without subcutaneous injection ports for treatment of cancer pain. Anesth Analg. 1994; 78:94–100. PMID: 8267188.
Article17. Carde P, Cosset-Delaigue MF, Laplanche A, Chareau I. Classical external indwelling central venous catheter versus totally implanted venous access systems for chemotherapy administration: a randomized trial in 100 patients with solid tumors. Eur J Cancer Clin Oncol. 1989; 25:939–944. PMID: 2666137.
Article18. Orser B. Obstetrical epidural anaesthesia in a Canadian outpost hospital. Can J Anaesth. 1988; 35:503–506. PMID: 3168135.
Article19. Prince G, McGregor D. Obstetric epidural test doses. A reappraisal. Anaesthesia. 1986; 41:1240–1250. PMID: 3544942.20. Guay J. The epidural test dose: a review. Anesth Analg. 2006; 102:921–929. PMID: 16492853.
Article21. de Leon-Casasola OA. Interventional procedures for cancer pain management: when are they indicated? Cancer Invest. 2004; 22:630–642. PMID: 15565820.
Article22. Bedder MD, Burchiel K, Larson A. Cost analysis of two implantable narcotic delivery systems. J Pain Symptom Manage. 1991; 6:368–373. PMID: 1908884.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Continuous Intraventricular Morphine Infusion for Control of Pain in Terminal Cancer Patients
- Mananagement of Cancer Pain Using Portable Infusor
- Cancer Pain Management by Continuous Epidural Morphine Infusion via Subcutaneous Tunneling
- Terminal Cancer Pain Management by Tunnelled Epidural Catheter
- Analgesic Effects of Epidural Morphine on Cancer-related Pain