Korean J Urol.
2014 Dec;55(12):780-788. 10.4111/kju.2014.55.12.780.
Current Status of Cryotherapy for Prostate and Kidney Cancer
- Affiliations
-
- 1Department of Urology, Korea University Anam Hospital, Seoul, Korea. mdksh@korea.ac.kr
- KMID: 2070091
- DOI: http://doi.org/10.4111/kju.2014.55.12.780
Abstract
- In terms of treating diseases, minimally invasive treatment has become a key element in reducing perioperative complications. Among the various minimally invasive treatments, cryotherapy is often used in urology to treat various types of cancers, especially prostate cancer and renal cancer. In prostate cancer, the increased incidence of low-risk, localized prostate cancer has made minimally invasive treatment modalities an attractive option. Focal cryotherapy for localized unilateral disease offers the added benefit of minimal morbidities. In renal cancer, owing to the increasing utilization of cross-sectional imaging, nearly 70% of newly detected renal masses are stage T1a, making them more susceptible to minimally invasive nephron-sparing therapies including laparoscopic and robotic partial nephrectomy and ablative therapies. This article reviews the various outcomes of cryotherapy compared with other treatments and the possible uses of cryotherapy in surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Efficacy and Safety of Robotic Procedures Performed Using the da Vinci Robotic Surgical System at a Single Institute in Korea: Experience with 10000 Cases
Dong Hoon Koh, Won Sik Jang, Jae Won Park, Won Sik Ham, Woong Kyu Han, Koon Ho Rha, Young Deuk Choi
Yonsei Med J. 2018;59(8):975-981. doi: 10.3349/ymj.2018.59.8.975.
Reference
-
1. Korpan NN. A history of cryosurgery: its development and future. J Am Coll Surg. 2007; 204:314–324.2. Arnott J. Practical illustrations of the remedial efficacy of a very low or anaesthetic temperature. I. In cancer. Lancet. 1850; 56:257–259.3. White AC. Liquid air: its application in medicine and surgery. Med Rec. 1899; 56:109–112.4. Cooper IS, Lee AS, Steininger C. Cryostatic congelation: a system for producing a limited, controlled region of cooling or freezing of biologic tissues. J Nerv Ment Dis. 1961; 133:259–263.5. Cooper IS. Cryogenic surgery of the basal ganglia. JAMA. 1962; 181:600–604.6. Gonder MJ, Soanes WA, Smith V. Experimental prostate cryosurgery. Invest Urol. 1964; 1:610–619.7. Gonder MJ, Soanes WA, Shulman S. Cryosurgical treatment of the prostate. Invest Urol. 1966; 3:372–378.8. Zacarian SA, Adham MI. Cryotherapy of cutaneous malignancy. Cryobiology. 1966; 2:212–218.9. Crisp WE, Asadourian L, Romberger W. Application of cryosurgery to gynecologic malignancy. Obstet Gynecol. 1967; 30:668–673.10. Pandey SK, Milverton EJ, Maloof AJ. A tribute to Charles David Kelman MD: ophthalmologist, inventor and pioneer of phacoemulsification surgery. Clin Experiment Ophthalmol. 2004; 32:529–533.11. Korpan NN. Basics of cryosurgery. Wien: Springer Verlag Wien;2001.12. Onik GM, Cohen JK, Reyes GD, Rubinsky B, Chang Z, Baust J. Transrectal ultrasound-guided percutaneous radical cryosurgical ablation of the prostate. Cancer. 1993; 72:1291–1299.13. Ritch CR, Katz AE. Prostate cryotherapy: current status. Curr Opin Urol. 2009; 19:177–181.14. Whittaker DK. Mechanisms of tissue destruction following cryosurgery. Ann R Coll Surg Engl. 1984; 66:313–318.15. Hoffmann NE, Bischof JC. The cryobiology of cryosurgical injury. Urology. 2002; 60:2 Suppl 1. 40–49.16. Sindelar WF, Javadpour N, Bagley DH. Histological and ultrastructural changes in rat kidney after cryosurgery. J Surg Oncol. 1981; 18:363–379.17. Jones JS, Rewcastle JC, Donnelly BJ, Lugnani FM, Pisters LL, Katz AE. Whole gland primary prostate cryoablation: initial results from the cryo on-line data registry. J Urol. 2008; 180:554–558.18. Wilt TJ, MacDonald R, Rutks I, Shamliyan TA, Taylor BC, Kane RL. Systematic review: comparative effectiveness and harms of treatments for clinically localized prostate cancer. Ann Intern Med. 2008; 148:435–448.19. Chin JL, Ng CK, Touma NJ, Pus NJ, Hardie R, Abdelhady M, et al. Randomized trial comparing cryoablation and external beam radiotherapy for T2C-T3B prostate cancer. Prostate Cancer Prostatic Dis. 2008; 11:40–45.20. Mouraviev V, Polascik TJ. Update on cryotherapy for prostate cancer in 2006. Curr Opin Urol. 2006; 16:152–156.21. Cohen JK, Miller RJ Jr, Ahmed S, Lotz MJ, Baust J. Ten-year biochemical disease control for patients with prostate cancer treated with cryosurgery as primary therapy. Urology. 2008; 71:515–518.22. Han KR, Cohen JK, Miller RJ, Pantuck AJ, Freitas DG, Cuevas CA, et al. Treatment of organ confined prostate cancer with third generation cryosurgery: preliminary multicenter experience. J Urol. 2003; 170(4 Pt 1):1126–1130.23. Hubosky SG, Fabrizio MD, Schellhammer PF, Barone BB, Tepera CM, Given RW. Single center experience with third-generation cryosurgery for management of organ-confined prostate cancer: critical evaluation of short-term outcomes, complications, and patient quality of life. J Endourol. 2007; 21:1521–1531.24. De Meerleer GO, Fonteyne VH, Vakaet L, Villeirs GM, Denoyette L, Verbaeys A, et al. Intensity-modulated radiation therapy for prostate cancer: late morbidity and results on biochemical control. Radiother Oncol. 2007; 82:160–166.25. Zapatero A, Minguez R, Nieto S, Martin de, Garcia-Vicente F. Post-treatment prostate biopsies in the era of threedimensional conformal radiotherapy: what can they teach us? Eur Urol. 2009; 55:902–909.26. Stephenson AJ, Scardino PT, Bianco FJ Jr, DiBlasio CJ, Fearn PA, Eastham JA. Morbidity and functional outcomes of salvage radical prostatectomy for locally recurrent prostate cancer after radiation therapy. J Urol. 2004; 172(6 Pt 1):2239–2243.27. Izawa JI, Perrotte P, Greene GF, Scott S, Levy L, McGuire E, et al. Local tumor control with salvage cryotherapy for locally recurrent prostate cancer after external beam radiotherapy. J Urol. 2001; 165:867–870.28. Pisters LL, Rewcastle JC, Donnelly BJ, Lugnani FM, Katz AE, Jones JS. Salvage prostate cryoablation: initial results from the cryo on-line data registry. J Urol. 2008; 180:559–563.29. Chin JL, Touma N, Pautler SE, Guram KS, Bella AJ, Downey DB, et al. Serial histopathology results of salvage cryoablation for prostate cancer after radiation failure. J Urol. 2003; 170(4 Pt 1):1199–1202.30. Izawa JI, Busby JE, Morganstern N, Vakar-Lopez F, Scott SM, Pisters LL. Histological changes in prostate biopsies after salvage cryotherapy: effect of chronology and the method of biopsy. BJU Int. 2006; 98:554–558.31. Ng CK, Moussa M, Downey DB, Chin JL. Salvage cryoablation of the prostate: followup and analysis of predictive factors for outcome. J Urol. 2007; 178(4 Pt 1):1253–1257.32. Ghafar MA, Johnson CW, De La, Benson MC, Bagiella E, Fatal M, et al. Salvage cryotherapy using an argon based system for locally recurrent prostate cancer after radiation therapy: the Columbia experience. J Urol. 2001; 166:1333–1337.33. Ismail M, Ahmed S, Kastner C, Davies J. Salvage cryotherapy for recurrent prostate cancer after radiation failure: a prospective case series of the first 100 patients. BJU Int. 2007; 100:760–764.34. Long JP, Fallick ML, LaRock DR, Rand W. Preliminary outcomes following cryosurgical ablation of the prostate in patients with clinically localized prostate carcinoma. J Urol. 1998; 159:477–484.35. Han KR, Belldegrun AS. Third-generation cryosurgery for primary and recurrent prostate cancer. BJU Int. 2004; 93:14–18.36. Anastasiadis AG, Sachdev R, Salomon L, Ghafar MA, Stisser BC, Shabsigh R, et al. Comparison of health-related quality of life and prostate-associated symptoms after primary and salvage cryotherapy for prostate cancer. J Cancer Res Clin Oncol. 2003; 129:676–682.37. Babaian RJ, Donnelly B, Bahn D, Baust JG, Dineen M, Ellis D, et al. Best practice statement on cryosurgery for the treatment of localized prostate cancer. J Urol. 2008; 180:1993–2004.38. Onik G, Vaughan D, Lotenfoe R, Dineen M, Brady J. The "male lumpectomy": focal therapy for prostate cancer using cryoablation results in 48 patients with at least 2-year follow-up. Urol Oncol. 2008; 26:500–505.39. Abern MR, Tsivian M, Polascik TJ. Focal therapy of prostate cancer: evidence-based analysis for modern selection criteria. Curr Urol Rep. 2012; 13:160–169.40. Bomers JG, Sedelaar JP, Barentsz JO, Futterer JJ. MRI-guided interventions for the treatment of prostate cancer. AJR Am J Roentgenol. 2012; 199:714–720.41. Bozzini G, Colin P, Nevoux P, Villers A, Mordon S, Betrouni N. Focal therapy of prostate cancer: energies and procedures. Urol Oncol. 2013; 31:155–167.42. Onik G, Narayan P, Vaughan D, Dineen M, Brunelle R. Focal "nerve-sparing" cryosurgery for treatment of primary prostate cancer: a new approach to preserving potency. Urology. 2002; 60:109–114.43. Ward JF, Jones JS. Focal cryotherapy for localized prostate cancer: a report from the national Cryo On-Line Database (COLD) Registry. BJU Int. 2012; 109:1648–1654.44. Lambert EH, Bolte K, Masson P, Katz AE. Focal cryosurgery: encouraging health outcomes for unifocal prostate cancer. Urology. 2007; 69:1117–1120.45. Ellis DS, Manny TB Jr, Rewcastle JC. Focal cryosurgery followed by penile rehabilitation as primary treatment for localized prostate cancer: initial results. Urology. 2007; 70:6 Suppl. 9–15.46. Bahn D, de Castro Abreu AL, Gill IS, Hung AJ, Silverman P, Gross ME, et al. Focal cryotherapy for clinically unilateral, low-intermediate risk prostate cancer in 73 men with a median follow-up of 3.7 years. Eur Urol. 2012; 62:55–63.47. Uchida M, Imaide Y, Sugimoto K, Uehara H, Watanabe H. Percutaneous cryosurgery for renal tumours. Br J Urol. 1995; 75:132–136.48. Woldrich JM, Palazzi K, Stroup SP, Sur RL, Parsons JK, Chang D, et al. Trends in the surgical management of localized renal masses: thermal ablation, partial and radical nephrectomy in the USA, 1998-2008. BJU Int. 2013; 111:1261–1268.49. Berger A, Kamoi K, Gill IS, Aron M. Cryoablation for renal tumors: current status. Curr Opin Urol. 2009; 19:138–142.50. Kunkle DA, Egleston BL, Uzzo RG. Excise, ablate or observe: the small renal mass dilemma--a meta-analysis and review. J Urol. 2008; 179:1227–1233.51. Weight CJ, Kaouk JH, Hegarty NJ, Remer EM, O'Malley CM, Lane BR, et al. Correlation of radiographic imaging and histopathology following cryoablation and radio frequency ablation for renal tumors. J Urol. 2008; 179:1277–1281.52. Klatte T, Grubmuller B, Waldert M, Weibl P, Remzi M. Laparoscopic cryoablation versus partial nephrectomy for the treatment of small renal masses: systematic review and cumulative analysis of observational studies. Eur Urol. 2011; 60:435–443.53. Tsivian M, Lyne JC, Mayes JM, Mouraviev V, Kimura M, Polascik TJ. Tumor size and endophytic growth pattern affect recurrence rates after laparoscopic renal cryoablation. Urology. 2010; 75:307–310.54. Aron M, Kamoi K, Remer E, Berger A, Desai M, Gill I. Laparoscopic renal cryoablation: 8-year, single surgeon outcomes. J Urol. 2010; 183:889–895.55. Tanagho YS, Roytman TM, Bhayani SB, Kim EH, Benway BM, Gardner MW, et al. Laparoscopic cryoablation of renal masses: single-center long-term experience. Urology. 2012; 80:307–314.56. Desai MM, Aron M, Gill IS. Laparoscopic partial nephrectomy versus laparoscopic cryoablation for the small renal tumor. Urology. 2005; 66:5 Suppl. 23–28.57. O'Malley RL, Berger AD, Kanofsky JA, Phillips CK, Stifelman M, Taneja SS. A matched-cohort comparison of laparoscopic cryoablation and laparoscopic partial nephrectomy for treating renal masses. BJU Int. 2007; 99:395–398.58. Ko YH, Park HS, Moon du G, Lee JG, Kim JJ, Yoon DK, et al. A matched-cohort comparison of laparoscopic renal cryoablation using ultra-thin cryoprobes with open partial nephrectomy for the treatment of small renal cell carcinoma. Cancer Res Treat. 2008; 40:184–189.59. Tsivian M, Caso J, Kimura M, Polascik TJ. Renal function outcomes after laparoscopic renal cryoablation. J Endourol. 2011; 25:1287–1291.60. Haber GP, Lee MC, Crouzet S, Kamoi K, Gill IS. Tumour in solitary kidney: laparoscopic partial nephrectomy vs laparoscopic cryoablation. BJU Int. 2012; 109:118–124.61. Panumatrassamee K, Kaouk JH, Autorino R, Lenis AT, Laydner H, Isac W, et al. Cryoablation versus minimally invasive partial nephrectomy for small renal masses in the solitary kidney: impact of approach on functional outcomes. J Urol. 2013; 189:818–822.62. Turna B, Kaouk JH, Frota R, Stein RJ, Kamoi K, Gill IS, et al. Minimally invasive nephron sparing management for renal tumors in solitary kidneys. J Urol. 2009; 182:2150–2157.63. Wyler SF, Sulser T, Ruszat R, Weltzien B, Forster TH, Provenzano M, et al. Intermediate-term results of retroperitoneoscopy-assisted cryotherapy for small renal tumours using multiple ultrathin cryoprobes. Eur Urol. 2007; 51:971–979.64. Weld KJ, Figenshau RS, Venkatesh R, Bhayani SB, Ames CD, Clayman RV, et al. Laparoscopic cryoablation for small renal masses: three-year follow-up. Urology. 2007; 69:448–451.65. Wright AD, Turk TM, Nagar MS, Phelan MW, Perry KT. Endophytic lesions: a predictor of failure in laparoscopic renal cryoablation. J Endourol. 2007; 21:1493–1496.66. Derweesh IH, Malcolm JB, Diblasio CJ, Giem A, Rewcastle JC, Wake RW, et al. Single center comparison of laparoscopic cryoablation and CT-guided percutaneous cryoablation for renal tumors. J Endourol. 2008; 22:2461–2467.67. Ko YH, Choi H, Kang SG, Park HS, Lee JG, Kim JJ, et al. Efficacy of laparoscopic renal cryoablation as an alternative treatment for small renal mass in patients with poor operability: experience from the Korean single center. J Laparoendosc Adv Surg Tech A. 2010; 20:339–345.68. Guazzoni G, Cestari A, Buffi N, Lughezzani G, Nava L, Cardone G, et al. Oncologic results of laparoscopic renal cryoablation for clinical T1a tumors: 8 years of experience in a single institution. Urology. 2010; 76:624–629.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Diagnostic Value of Prostate-specific Antigen and the of Routine Laboratory Examination for Early Detection
- Chemoprevention
- Diagnosis of Prostate Cancer
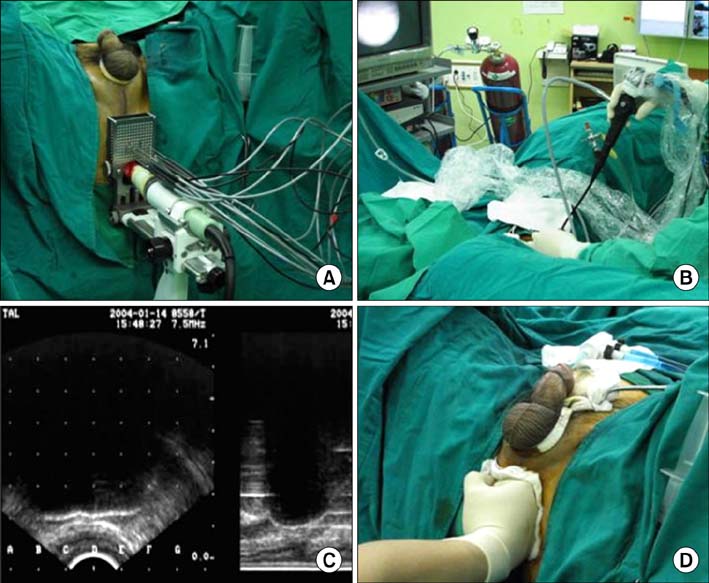
- Third-generation Cryosurgery for Prostate Cancer Patient with a Penile Prosthesis
- Epidemiological evidences on overdiagnosis of prostate and kidney cancers in Korean