Yonsei Med J.
2015 Mar;56(2):519-528. 10.3349/ymj.2015.56.2.519.
Clinical Features and Computed Tomography Characteristics of Non-Klebsiella pneumoniae Liver Abscesses in Elderly (>65 Years) and Nonelderly Patients
- Affiliations
-
- 1Department of Radiology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China. weichou.chang@gmail.com
- 2Division of General Surgery, Department of Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China.
- 3Department of Emergency Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China.
- KMID: 2070033
- DOI: http://doi.org/10.3349/ymj.2015.56.2.519
Abstract
- PURPOSE
To compare the clinical and computed tomography (CT) appearances of liver abscesses caused by non-Klebsiella pneumoniae bacterial pathogens in elderly and nonelderly patients.
MATERIALS AND METHODS
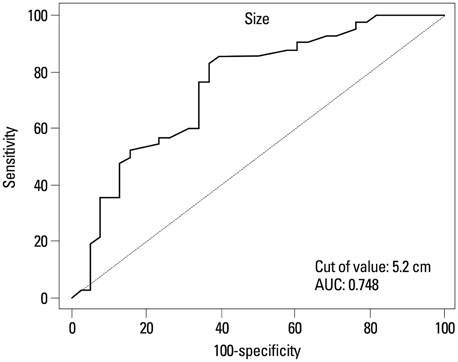
Eighty patients with confirmed non-Klebsiella pneumoniae liver abscesses (non-KPLAs) were enrolled and divided into two age groups: elderly (age > or =65 years, n=42) and nonelderly (age <65 years, n=38). Diagnosis of non-KPLA was established by pus and/or blood culture. We compared clinical presentations, outcomes, and CT characteristics of the two groups, and performed multivariate analysis for significant variables and receiver-operating-characteristic analysis to determine the cutoff value of abscess diameter for predicting non-KPLA.
RESULTS
Elderly patients with non-KPLA were associated with a longer hospital stay (p<0.01). Regarding etiology, biliary sources had a strong association in the elderly group (p<0.01), and chronic liver diseases were related to the nonelderly group (p<0.01). Non-KPLAs (52.5%) tended to show a large, multiloculated appearance in the elderly group and were associated with bile duct dilatation (p<0.01), compared with the nonelderly group. The abscess diameter (cutoff value, 5.2 cm; area under the curve, 0.78) between the two groups was predicted. In multivariate analysis, underlying biliary tract disease [odds ratio (OR), 3.58, p<0.05], abscess diameter (OR, 2.40, p<0.05), and multiloculated abscess (OR, 1.19, p<0.01) independently predicted elderly patients with non-KPLA.
CONCLUSION
In the elderly patients with non-KPLA, a large, multiloculated abscess with a diameter greater than 5.2 cm was the predominant imaging feature.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Bacterial Infections/*complications/*radiography
Female
Humans
Klebsiella Infections/microbiology
Klebsiella pneumoniae
Length of Stay
Liver Abscess/complications/microbiology/*radiography
Logistic Models
Male
Microscopy
Middle Aged
Multivariate Analysis
ROC Curve
Retrospective Studies
Tomography, X-Ray Computed/*methods
Figure
Reference
-
1. Foo NP, Chen KT, Lin HJ, Guo HR. Characteristics of pyogenic liver abscess patients with and without diabetes mellitus. Am J Gastroenterol. 2010; 105:328–335.
Article2. Lee NK, Kim S, Lee JW, Jeong YJ, Lee SH, Heo J, et al. CT differentiation of pyogenic liver abscesses caused by Klebsiella pneumoniae vs non-Klebsiella pneumoniae. Br J Radiol. 2011; 84:518–525.
Article3. Alsaif HS, Venkatesh SK, Chan DS, Archuleta S. CT appearance of pyogenic liver abscesses caused by Klebsiella pneumoniae. Radiology. 2011; 260:129–138.
Article4. Yang CC, Yen CH, Ho MW, Wang JH. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect. 2004; 37:176–184.5. Lederman ER, Crum NF. Pyogenic liver abscess with a focus on Klebsiella pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics. Am J Gastroenterol. 2005; 100:322–331.
Article6. Law ST, Li KK. Older age as a poor prognostic sign in patients with pyogenic liver abscess. Int J Infect Dis. 2013; 17:e177–e184.
Article7. Chen SC, Lee YT, Yen CH, Lai KC, Jeng LB, Lin DB, et al. Pyogenic liver abscess in the elderly: clinical features, outcomes and prognostic factors. Age Ageing. 2009; 38:271–276.
Article8. Alvarez JA, González JJ, Baldonedo RF, Sanz L, Junco A, Rodrfíguez JL, et al. Pyogenic liver abscesses: a comparison of older and younger patients. HPB (Oxford). 2001; 3:201–206.
Article9. Kang SC, Hwang SJ. Impact of advanced age on inpatients with pyogenic liver abscess in Taiwan: a nationwide claim-based analysis. J Chin Med Assoc. 2011; 74:539–543.
Article10. Tan YM, Chung AY, Chow PK, Cheow PC, Wong WK, Ooi LL, et al. An appraisal of surgical and percutaneous drainage for pyogenic liver abscesses larger than 5 cm. Ann Surg. 2005; 241:485–490.
Article11. Lee CH, Leu HS, Wu TS, Su LH, Liu JW. Risk factors for spontaneous rupture of liver abscess caused by Klebsiella pneumoniae. Diagn Microbiol Infect Dis. 2005; 52:79–84.
Article12. Liao WI, Tsai SH, Yu CY, Huang GS, Lin YY, Hsu CW, et al. Pyogenic liver abscess treated by percutaneous catheter drainage: MDCT measurement for treatment outcome. Eur J Radiol. 2012; 81:609–615.
Article13. Tazawa J, Sakai Y, Maekawa S, Ishida Y, Maeda M, Marumo F, et al. Solitary and multiple pyogenic liver abscesses: characteristics of the patients and efficacy of percutaneous drainage. Am J Gastroenterol. 1997; 92:271–274.14. Chou FF, Sheen-Chen SM, Chen YS, Chen MC. Single and multiple pyogenic liver abscesses: clinical course, etiology, and results of treatment. World J Surg. 1997; 21:384–388.
Article15. Liu CH, Gervais DA, Hahn PF, Arellano RS, Uppot RN, Mueller PR. Percutaneous hepatic abscess drainage: do multiple abscesses or multiloculated abscesses preclude drainage or affect outcome? J Vasc Interv Radiol. 2009; 20:1059–1065.
Article16. Barakate MS, Stephen MS, Waugh RC, Gallagher PJ, Solomon MJ, Storey DW, et al. Pyogenic liver abscess: a review of 10 years' experience in management. Aust N Z J Surg. 1999; 69:205–209.
Article17. Lam YH, Wong SK, Lee DW, Lau JY, Chan AC, Yiu RY, et al. ERCP and pyogenic liver abscess. Gastrointest Endosc. 1999; 50:340–344.
Article18. Walsh RM. Innovations in treating the elderly who have biliary and pancreatic disease. Clin Geriatr Med. 2006; 22:545–558.
Article19. Mølle I, Thulstrup AM, Jepsen P, Sørensen HT, Vilstrup H. Liver cirrhosis is risk factor for pyogenic liver abscesses. BMJ. 2001; 323:52–53.20. Tarantino G, Finelli C. What about non-alcoholic fatty liver disease as a new criterion to define metabolic syndrome? World J Gastroenterol. 2013; 19:3375–3384.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Klebsiella Pneumoniae Multi-organ Abscesses not Accompanied by Liver Abscesses: A Case Report
- Lower Leg Abscess in Klebsiella pneumoniae Invasive Syndrome Caused by Hypervirulent Klebsiella pneumoniae: A Case Report
- Two Cases of Bilateral Endogenous Klebsiella pneumoniae Endophthalmitis in Primary Klebsiella pneumoniae Liver Abscess Patients
- A clinical study on pyogenic liver abscesses: the changes in the clinical features during the recent 12 years
- Metastatic endophthalmitis and thyroid abscess complicating Klebsiella pneumoniae liver abscess