J Korean Med Sci.
2014 Dec;29(12):1632-1638. 10.3346/jkms.2014.29.12.1632.
Clinical Value of Endobronchial Ultrasound Findings for Predicting Nodal Metastasis in Patients with Suspected Lymphadenopathy: A Prospective Study
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, The Armed Forces Capital Hospital, Seongnam, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kj2011.lee@gmail.com
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2069951
- DOI: http://doi.org/10.3346/jkms.2014.29.12.1632
Abstract
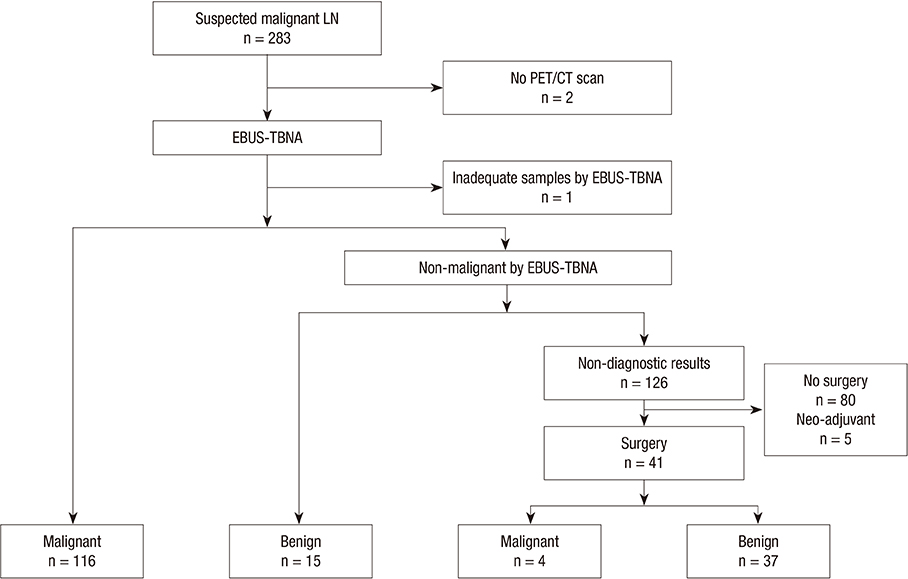
- We evaluated whether sonographic findings can provide additional diagnostic yield in endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), and can more accurately predict nodal metastasis than chest computed tomography (CT) or positron emission tomography (PET)/CT scans. EBUS-TBNA was performed in 146 prospectively recruited patients with suspected thoracic lymph node involvement on chest CT and PET/CT from June 2012 to January 2013. Diagnostic yields of EBUS finding categories as a prediction model for metastasis were evaluated and compared with findings of chest CT, PET/CT, and EBUS-TBNA. In total, 172 lymph nodes were included in the analysis: of them, 120 were malignant and 52 were benign. The following four EBUS findings were predictive of metastasis: nodal size > or =10 mm, round shape, heterogeneous echogenicity, and absence of central hilar structure. A single EBUS finding did not have sufficient diagnostic yield; however, when the lymph node had any one of the predictive factors on EBUS, the diagnostic yields for metastasis were higher than for chest CT and PET/CT, with a sensitivity of 99.1% and negative predictive value of 83.3%. When any one of predictive factors is observed on EBUS, subsequent TBNA should be considered, which may provide a higher diagnostic yield than chest CT or PET/CT.
MeSH Terms
-
Aged
Bronchi
Endoscopic Ultrasound-Guided Fine Needle Aspiration/*methods
Endosonography/*methods
Female
Humans
Lymph Nodes/*pathology/ultrasonography
Lymphatic Diseases/*pathology/ultrasonography
Lymphatic Metastasis
Male
Middle Aged
Prospective Studies
Reproducibility of Results
Sensitivity and Specificity
Thoracic Neoplasms/*pathology/*secondary/ultrasonography
Figure
Reference
-
1. Jhun BW, Park HY, Jeon K, Koh WJ, Suh GY, Chung MP, Kim H, Kwon OJ, Han J, Um SW. Nodal stations and diagnostic performances of endobronchial ultrasound-guided transbronchial needle aspiration in patients with non-small cell lung cancer. J Korean Med Sci. 2012; 27:46–51.2. Varela-Lema L, Fernandez-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: a systematic review. Eur Respir J. 2009; 33:1156–1164.3. Gu P, Zhao YZ, Jiang LY, Zhang W, Xin Y, Han BH. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur J Cancer. 2009; 45:1389–1396.4. Adams K, Shah PL, Edmonds L, Lim E. Test performance of endobronchial ultrasound and transbronchial needle aspiration biopsy for mediastinal staging in patients with lung cancer: systematic review and meta-analysis. Thorax. 2009; 64:757–762.5. Joo H, Kim HR, Oh YM, Kim YH, Shim TS, Kim D-K, Park SI, Kim WS, Kim DS, Choi CM. The efficacy of endobronchial ultrasound-guided transbronchial needle aspiration in mediastinal staging of non-small cell lung cancer in a university hospital. Tuberc Respir Dis. 2011; 71:180–187.6. Kang HJ, Hwangbo B. Technical aspects of endobronchial ultrasound-guided transbronchial needle aspiration. Tuberc Respir Dis (Seoul). 2013; 75:135–139.7. Ernst A, Eberhardt R, Krasnik M, Herth FJ. Efficacy of endobronchial ultrasound-guided transbronchial needle aspiration of hilar lymph nodes for diagnosing and staging cancer. J Thorac Oncol. 2009; 4:947–950.8. Schmid-Bindert G, Jiang H, Kähler G, Saur J, Henzler T, Wang H, Ren S, Zhou C, Pilz LR. Predicting malignancy in mediastinal lymph nodes by endobronchial ultrasound: a new ultrasound scoring system. Respirology. 2012; 17:1190–1198.9. Fujiwara T, Yasufuku K, Nakajima T, Chiyo M, Yoshida S, Suzuki M, Shibuya K, Hiroshima K, Nakatani Y, Yoshino I. The utility of sonographic features during endobronchial ultrasound-guided transbronchial needle aspiration for lymph node staging in patients with lung cancer: a standard endobronchial ultrasound image classification system. Chest. 2010; 138:641–647.10. Nakajima T, Anayama T, Shingyoji M, Kimura H, Yoshino I, Yasufuku K. Vascular image patterns of lymph nodes for the prediction of metastatic disease during EBUS-TBNA for mediastinal staging of lung cancer. J Thorac Oncol. 2012; 7:1009–1014.11. Memoli JS, El-Bayoumi E, Pastis NJ, Tanner NT, Gomez M, Huggins JT, Onicescu G, Garrett-Mayer E, Armeson K, Taylor KK, et al. Using endobronchial ultrasound features to predict lymph node metastasis in patients with lung cancer. Chest. 2011; 140:1550–1556.12. Roberts SA, Mahon BS, Evans R. Coagulation necrosis in malignant mediastinal nodes on endoscopic ultrasound: a new endosonographic sign. Clin Radiol. 2005; 60:587–591.13. Schmulewitz N, Wildi SM, Varadarajulu S, Roberts S, Hawes RH, Hoffman BJ, Durkalski V, Silvestri GA, Block MI, Reed C, et al. Accuracy of EUS criteria and primary tumor site for identification of mediastinal lymph node metastasis from non-small-cell lung cancer. Gastrointest Endosc. 2004; 59:205–212.14. Eloubeidi MA, Wallace MB, Reed CE, Hadzijahic N, Lewin DN, Van Velse A, Leveen MB, Etemad B, Matsuda K, Patel RS, et al. The utility of EUS and EUS-guided fine needle aspiration in detecting celiac lymph node metastasis in patients with esophageal cancer: a single-center experience. Gastrointest Endosc. 2001; 54:714–719.15. Yang WT, Metreweli C. Colour Doppler flow in normal axillary lymph nodes. Br J Radiol. 1998; 71:381–383.16. Ahuja AT, Ying M. Sonographic evaluation of cervical lymph nodes. AJR Am J Roentgenol. 2005; 184:1691–1699.17. Bhutani MS, Hawes RH, Hoffman BJ. A comparison of the accuracy of echo features during endoscopic ultrasound (EUS) and EUS-guided fine-needle aspiration for diagnosis of malignant lymph node invasion. Gastrointest Endosc. 1997; 45:474–479.18. Catalano MF, Sivak MV Jr, Rice T, Gragg LA, Van Dam J. Endosonographic features predictive of lymph node metastasis. Gastrointest Endosc. 1994; 40:442–446.19. Lee N, Inoue K, Yamamoto R, Kinoshita H. Patterns of internal echoes in lymph nodes in the diagnosis of lung cancer metastasis. World J Surg. 1992; 16:986–993. discussion 93-4.20. Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, Choi JY, Kwon OJ, Shim YM, Kim S. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005; 236:1011–1019.21. Hong R, Halama J, Bova D, Sethi A, Emami B. Correlation of PET standard uptake value and CT window-level thresholds for target delineation in CT-based radiation treatment planning. Int J Radiat Oncol Biol Phys. 2007; 67:720–726.22. Lee HS, Lee GK, Lee HS, Kim MS, Lee JM, Kim HY, Nam BH, Zo JI, Hwangbo B. Real-time endobronchial ultrasound-guided transbronchial needle aspiration in mediastinal staging of non-small cell lung cancer: how many aspirations per target lymph node station? Chest. 2008; 134:368–374.23. Chen VK, Eloubeidi MA. Endoscopic ultrasound-guided fine needle aspiration is superior to lymph node echofeatures: a prospective evaluation of mediastinal and peri-intestinal lymphadenopathy. Am J Gastroenterol. 2004; 99:628–633.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT Findings of Cervical Lymphadenopathy: Differential Diagnosis
- Endobronchial Ultrasound-guided Transbronchial Needle Biopsy for Diagnosis of Mediastinal Lymphadenopathy in Patients with Extrathoracic Malignancy
- Endobronchial Metastases of Hepatocellular Carcinoma
- The First Pediatric Case of Intrathoracic Tuberculosis Lymphadenitis Diagnosed by Endobronchial Ultrasound Guided Transbronchial Needle Aspiration
- Nodal Stations and Diagnostic Performances of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in Patients with Non-Small Cell Lung Cancer