Korean J Urol.
2014 Nov;55(11):750-755. 10.4111/kju.2014.55.11.750.
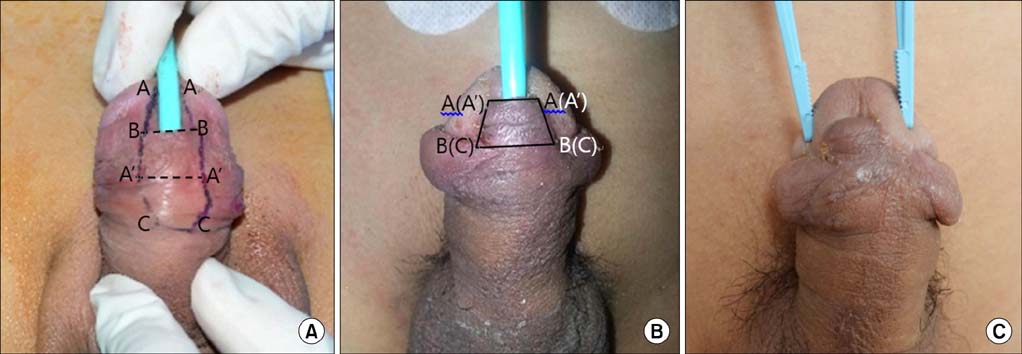
Urethroplasty by Use of Turnover Flaps (Modified Mathieu Procedure) for Distal Hypospadias Repair in Adolescents: Comparison With the Tubularized Incised Plate Procedure
- Affiliations
-
- 1Department of Urology, Kyungpook National University School of Medicine, Daegu, Korea. skchung@knu.ac.kr
- KMID: 2069918
- DOI: http://doi.org/10.4111/kju.2014.55.11.750
Abstract
- PURPOSE
The purpose of this study was to examine whether urethroplasty with a turnover flap, as an alternative method of distal hypospadias repair in adolescents, improves the outcome of surgery.
MATERIALS AND METHODS
Between January 2004 and December 2013, a total of 38 adolescents (aged 11-17 years) underwent distal hypospadias repair with either the tubularized incised plate (TIP) procedure (n=25) or the turnover flap procedure (n=13). The turnover flap procedure was performed with a proximal, ventral penile flap that was turned over to cover the urethral plate. Patient demographics, perioperative outcomes, complications, and postoperative uroflowmetry in each surgical group were analyzed retrospectively.
RESULTS
The patient demographics were similar in the two groups. There were no significant differences in perioperative outcomes between the groups, including mean operative time, duration of hospital stay, and urethral catheterization. The number of patients with at least one complication, including wound dehiscence, urethrocutaneous fistula, meatal stenosis, and urethral stricture, was lower in the turnover flap group (1/13, 7.7%) than in the TIP group (11/25, 44%, p=0.030). The incidence of meatal stenosis was lower in the turnover flap group (0/12, 0%) than in the TIP group (6/25, 24%). In postoperative uroflowmetry, the plateau-shaped curve rate was lower in the turnover flap group (1/12, 8.3%) than in the TIP group (5/19, 26.3%); the peak flow was higher (p=0.030).
CONCLUSIONS
The turnover flap procedure is clinically useful for repairing adolescent distal hypospadias because it offers lower complication rates and better functional outcomes than TIP.
Keyword
MeSH Terms
Figure
Reference
-
1. Cook A, Khoury AE, Neville C, Bagli DJ, Farhat WA, Pippi Salle JL. A multicenter evaluation of technical preferences for primary hypospadias repair. J Urol. 2005; 174:2354–2357.2. Snodgrass W, Koyle M, Manzoni G, Hurwitz R, Caldamone A, Ehrlich R. Tubularized incised plate hypospadias repair: results of a multicenter experience. J Urol. 1996; 156(2 Pt 2):839–841.3. Retik AB, Borer JG. Primary and reoperative hypospadias repair with the Snodgrass technique. World J Urol. 1998; 16:186–191.4. Sugarman ID, Trevett J, Malone PS. Tubularization of the incised urethral plate (Snodgrass procedure) for primary hypospadias surgery. BJU Int. 1999; 83:88–90.5. Chen SC, Yang SS, Hsieh CH, Chen YT. Tubularized incised plate urethroplasty for proximal hypospadias. BJU Int. 2000; 86:1050–1053.6. Elicevik M, Tireli G, Sander S. Tubularized incised plate urethroplasty: 5 years' experience. Eur Urol. 2004; 46:655–659.7. Dodson JL, Baird AD, Baker LA, Docimo SG, Mathews RI. Outcomes of delayed hypospadias repair: implications for decision making. J Urol. 2007; 178:278–281.8. Yildiz T, Tahtali IN, Ates DC, Keles I, Ilce Z. Age of patient is a risk factor for urethrocutaneous fistula in hypospadias surgery. J Pediatr Urol. 2013; 9(6 Pt A):900–903.9. Eassa W, Jednak R, Capolicchio JP, Brzezinski A, El-Sherbiny M. Risk factors for re-operation following tubularized incised plate urethroplasty: a comprehensive analysis. Urology. 2011; 77:716–720.10. Snodgrass W. Tubularized, incised plate urethroplasty for distal hypospadias. J Urol. 1994; 151:464–465.11. Snodgrass WT. Tubularized incised plate (TIP) hypospadias repair. Urol Clin North Am. 2002; 29:285–290.12. Baskin LS, Duckett JW. Dorsal tunica albuginea plication for hypospadias curvature. J Urol. 1994; 151:1668–1671.13. Braga LH, Lorenzo AJ, Salle JL. Tubularized incised plate urethroplasty for distal hypospadias: a literature review. Indian J Urol. 2008; 24:219–225.14. Elbakry A. Further experience with the tubularized-incised urethral plate technique for hypospadias repair. BJU Int. 2002; 89:291–294.15. Toguri AG, Uchida T, Bee DE. Pediatric uroflow rate nomograms. J Urol. 1982; 127:727–731.16. Marte A, Di Iorio G, De Pasquale M, Cotrufo AM, Di Meglio D. Functional evaluation of tubularized-incised plate repair of midshaft-proximal hypospadias using uroflowmetry. BJU Int. 2001; 87:540–543.17. de Jong TP, Boemers TM. Improved Mathieu repair for coronal and distal shaft hypospadias with moderate chordee. Br J Urol. 1993; 72:972–974.18. ElGanainy EO, Hameed DA, Abdelsalam YM, Abdelaziz MA. Prepuce preserving versus conventional Mathieu urethroplasty for distal hypospadias: a prospective randomized study. J Pediatr Urol. 2012; 8:264–267.19. Nezami BG, Mahboubi AH, Tanhaeivash R, Tourchi A, Kajbafzadeh AM. Hypospadias repair and glans augmentation using a modified Mathieu technique. Pediatr Surg Int. 2010; 26:299–303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Transverse Preputial Island Flap, Onlay Island Flap and Tubularized Incised Plate Urethroplasty for Proximal Hypospadias
- Outcome of Tubularized Incised Plate Urethroplasty for Correction of Hypospadias
- Outcome of Tubularized Incised Plate (TIP) Urethroplasty for Hypospadias Reoperation
- Comparison of the Surgical Outcome between Onlay Island Flap and Tubularized Incised Plate Urethroplasty in Hypospadias Repair
- Tubularized Incised-plate Urethroplasty: Expanded Use in Primary and Repeat Surgery for Hypospadias