Infect Chemother.
2015 Jun;47(2):111-116. 10.3947/ic.2015.47.2.111.
Impact of an Antimicrobial Stewardship Program on Unnecessary Double Anaerobic Coverage Prescription
- Affiliations
-
- 1Department of Pharmacy, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. hbkimmd@snu.ac.kr
- 3Department of Internal medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2068995
- DOI: http://doi.org/10.3947/ic.2015.47.2.111
Abstract
- BACKGROUND
Co-administration of two or more antimicrobials with anti-anaerobic activity is not recommended except in certain circumstances. We therefore conducted an intervention to reduce unnecessary double anaerobic coverage (DAC) prescription.
MATERIALS AND METHODS
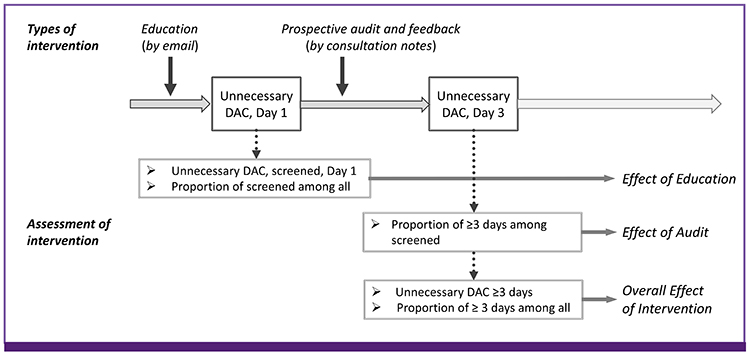
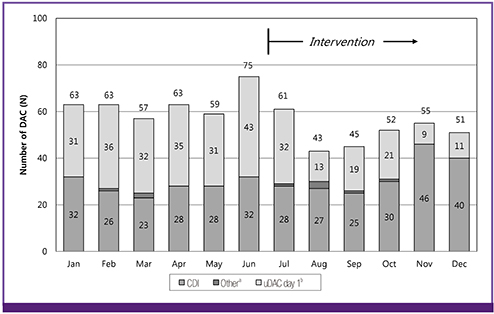
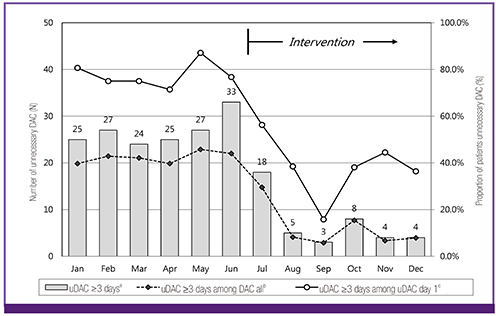
The intervention consisted of education using an institutional intranet and prospective audits and feedback provided through collaboration between a pharmacist and an infectious diseases physician in Seoul National University Bundang Hospital, a tertiary hospital in Seongnam, Republic of Korea, in 2013. The study period was 1 year which contained 6 months of pre-intervention period and 6 months of intervention period. To estimate the overall effect of the intervention, we compared the monthly number of patients receiving unnecessary DAC for more than 3 days and the proportion of patients receiving unnecessary DAC for more than 3 days among all patients receiving DAC.
RESULTS
The average monthly number of patients receiving unnecessary DAC for more than 3 days after screening decreased by 73.9% in the intervention period from 26.8 to 7.0. Wilcoxon rank sum test revealed there was a significant statistical difference in the monthly number of patients receiving unnecessary DAC for more than 3 days (P = 0.005). The proportion of patients receiving unnecessary DAC for more than 3 days after screening among all patients identified as receiving necessary or unnecessary DAC also decreased by 67.8% in the intervention period from 42.3% to 13.6% (P < 0.001).
CONCLUSION
The multidisciplinary antimicrobial stewardship program with combined methods reduced unnecessary DAC prescription successfully.
MeSH Terms
Figure
Cited by 3 articles
-
Impact of Intervention by an Antimicrobial Stewardship Team on Conversion from Intravenous to Oral Fluoroquinolones
Soh Mee Park, Hyung-sook Kim, Young Mi Jeong, Jung Hwa Lee, Eunsook Lee, Euni Lee, Kyoung-Ho Song, Hong Bin Kim, Eu Suk Kim
Infect Chemother. 2017;49(1):31-37. doi: 10.3947/ic.2017.49.1.31.Antimicrobial Stewardship with Intravenous to Oral Conversion and Future Directions of Antimicrobial Stewardship
Shin-Woo Kim
Infect Chemother. 2017;49(1):87-89. doi: 10.3947/ic.2017.49.1.87.Principles of selecting appropriate antimicrobial agents
Su-Mi Choi, Dong-Gun Lee
J Korean Med Assoc. 2019;62(6):335-344. doi: 10.5124/jkma.2019.62.6.335.
Reference
-
1. Kapoor K, Chandra M, Nag D, Paliwal JK, Gupta RC, Saxena RC. Evaluation of metronidazole toxicity: a prospective study. Int J Clin Pharmacol Res. 1999; 19:83–88.2. Kazmier FJ. A significant interaction between metronidazole and warfarin. Mayo Clin Proc. 1976; 51:782–784.3. Lucas GM, Lechtzin N, Puryear DW, Yau LL, Flexner CW, Moore RD. Vancomycin-resistant and vancomycin-susceptible enterococcal bacteremia: comparison of clinical features and outcomes. Clin Infect Dis. 1998; 26:1127–1133.
Article4. Brown KA, Khanafer N, Daneman N, Fisman DN. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother. 2013; 57:2326–2332.
Article5. Huttner B, Jones M, Rubin MA, Madaras-Kelly K, Nielson C, Goetz MB, Neuhauser MM, Samore MH. Double trouble: how big a problem is redundant anaerobic antibiotic coverage in Veterans Affairs medical centres? J Antimicrob Chemother. 2012; 67:1537–1539.
Article6. Rattanaumpawan P, Morales KH, Binkley S, Synnestvedt M, Weiner MG, Gasink LB, Fishman NO, Lautenbach E. Impact of antimicrobial stewardship programme changes on unnecessary double anaerobic coverage therapy. J Antimicrob Chemother. 2011; 66:2655–2658.
Article7. Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 2003; 163:972–978.
Article8. Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM. Infectious Diseases Society of America. Society for Healthcare Epidemiology of America. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007; 44:159–177.
Article9. Pollack LA, Srinivasan A. Core elements of hospital antibiotic stewardship programs from the Centers for Disease Control and Prevention. Clin Infect Dis. 2014; 59:Suppl 3. S97–S100.
Article10. Girotti MJ, Fodoruk S, Irvine-Meek J, Rotstein OD. Antibiotic handbook and pre-printed perioperative order forms for surgical antibiotic prophylaxis: do they work? Can J Surg. 1990; 33:385–388.11. Kim HI, Kim SW, Chang HH, Kim HB. A survey of antimicrobial stewardship programs in Korean hospitals. Korean J Med. 2014; 87:173–181.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Therapy and Antimicrobial Stewardship in Sepsis
- Antimicrobial Consumption as a Key Component of Antimicrobial Stewardship Programs: a Meaningful Movement toward Evidence-based Antimicrobial Stewardship of Validated Outcome Measures
- Antimicrobial Stewardship Program Focused on Prolonged Carbapenem Prescription
- Proper Antimicrobial Stewardship in Terms of Management of Drug Allergy
- Optimal antimicrobial therapy and antimicrobial stewardship in sepsis and septic shock