Pediatr Gastroenterol Hepatol Nutr.
2015 Sep;18(3):149-159. 10.5223/pghn.2015.18.3.149.
Pediatric Magnetic Resonance Enterography: Focused on Crohn's Disease
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul, Korea. kimws@snu.ac.kr
- 2Department of Radiology, Kyungpook National University Medical Center, Daegu, Korea.
- KMID: 2068791
- DOI: http://doi.org/10.5223/pghn.2015.18.3.149
Abstract
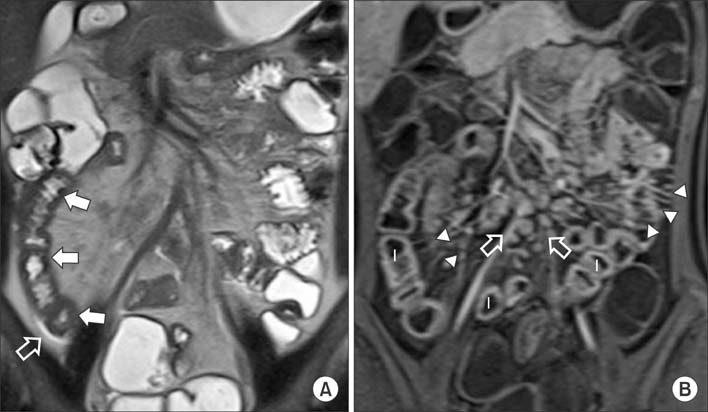
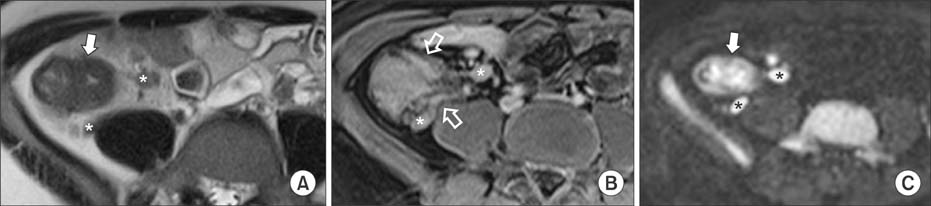
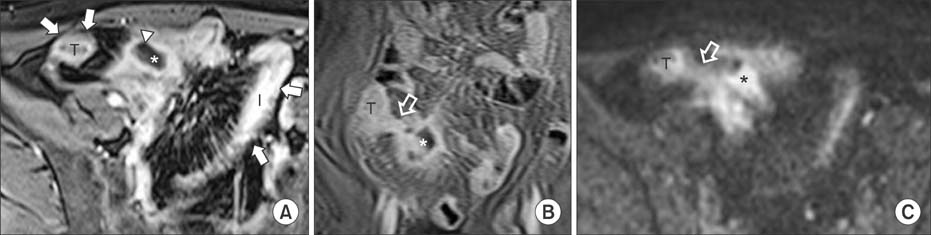
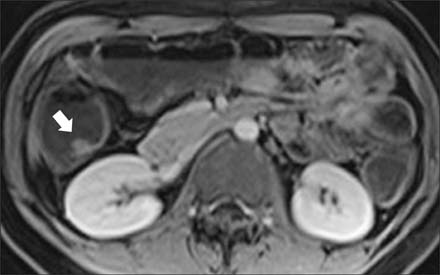
- Crohn's disease is a chronic idiopathic inflammatory disease of the intestines characterized by frequent relapse and remission. It often develops in children and adolescents, who are vulnerable to repeated exposure to ionizing radiations. Magnetic resonance enterography (MRE) is an increasingly important radiation-free imaging modality that is used to evaluate pediatric patients with Crohn's disease. MRE can evaluate extraluminal and extraintestinal abnormalities as well as the status of the bowel wall. In addition, MRE has an advantage in the evaluation of the small bowel involvement. MRE can be used for the initial diagnosis of Crohn's disease, and can aid in the assessment of disease activity and complications such as penetrating and fibrostenotic diseases. The aims of this article are to review the MRE technique for obtaining diagnostic and high-quality images and to discuss interpretations of imaging findings in patients with Crohn's disease.
Keyword
MeSH Terms
Figure
Reference
-
1. Leyendecker JR, Bloomfeld RS, DiSantis DJ, Waters GS, Mott R, Bechtold RE. MR enterography in the management of patients with Crohn disease. Radiographics. 2009; 29:1827–1846.
Article2. Day AS, Ledder O, Leach ST, Lemberg DA. Crohn's and colitis in children and adolescents. World J Gastroenterol. 2012; 18:5862–5869.
Article3. Tolan DJ, Greenhalgh R, Zealley IA, Halligan S, Taylor SA. MR enterographic manifestations of small bowel Crohn disease. Radiographics. 2010; 30:367–384.
Article4. Schreyer AG, Seitz J, Feuerbach S, Rogler G, Herfarth H. Modern imaging using computer tomography and magnetic resonance imaging for inflammatory bowel disease (IBD) AU1. Inflamm Bowel Dis. 2004; 10:45–54.
Article5. Desmond AN, O'Regan K, Curran C, McWilliams S, Fitzgerald T, Maher MM, et al. Crohn's disease: factors associated with exposure to high levels of diagnostic radiation. Gut. 2008; 57:1524–1529.
Article6. Lee SS, Kim AY, Yang SK, Chung JW, Kim SY, Park SH, et al. Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology. 2009; 251:751–761.
Article7. Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008; 247:64–79.
Article8. Froehlich JM, Waldherr C, Stoupis C, Erturk SM, Patak MA. MR motility imaging in Crohn's disease improves lesion detection compared with standard MR imaging. Eur Radiol. 2010; 20:1945–1951.
Article9. Del Vescovo R, Sansoni I, Caviglia R, Ribolsi M, Perrone G, Leoncini E, et al. Dynamic contrast enhanced magnetic resonance imaging of the terminal ileum: differentiation of activity of Crohn's disease. Abdom Imaging. 2008; 33:417–424.
Article10. Oto A, Fan X, Mustafi D, Jansen SA, Karczmar GS, Rubin DT, et al. Quantitative analysis of dynamic contrast enhanced MRI for assessment of bowel inflammation in Crohn's disease pilot study. Acad Radiol. 2009; 16:1223–1230.
Article11. Laghi A, Paolantonio P, Iafrate F, Altomari F, Miglio C, Passariello R. Oral contrast agents for magnetic resonance imaging of the bowel. Top Magn Reson Imaging. 2002; 13:389–396.
Article12. Lauenstein TC, Schneemann H, Vogt FM, Herborn CU, Ruhm SG, Debatin JF. Optimization of oral contrast agents for MR imaging of the small bowel. Radiology. 2003; 228:279–283.
Article13. Young BM, Fletcher JG, Booya F, Paulsen S, Fidler J, Johnson CD, et al. Head-to-head comparison of oral contrast agents for cross-sectional enterography: small bowel distention, timing, and side effects. J Comput Assist Tomogr. 2008; 32:32–38.
Article14. Kuehle CA, Ajaj W, Ladd SC, Massing S, Barkhausen J, Lauenstein TC. Hydro-MRI of the small bowel: effect of contrast volume, timing of contrast administration, and data acquisition on bowel distention. AJR Am J Roentgenol. 2006; 187:W375–W385.
Article15. Borthne AS, Abdelnoor M, Storaas T, Pierre-Jerome C, Kløw NE. Osmolarity: a decisive parameter of bowel agents in intestinal magnetic resonance imaging. Eur Radiol. 2006; 16:1331–1336.
Article16. Ajaj W, Goehde SC, Schneemann H, Ruehm SG, Debatin JF, Lauenstein TC. Dose optimization of mannitol solution for small bowel distension in MRI. J Magn Reson Imaging. 2004; 20:648–653.
Article17. Ajaj W, Goyen M, Schneemann H, Kuehle C, Nuefer M, Ruehm SG, et al. Oral contrast agents for small bowel distension in MRI: influence of the osmolarity for small bowel distention. Eur Radiol. 2005; 15:1400–1406.
Article18. Ajaj W, Goehde SC, Schneemann H, Ruehm SG, Debatin JF, Lauenstein TC. Oral contrast agents for small bowel MRI: comparison of different additives to optimize bowel distension. Eur Radiol. 2004; 14:458–464.
Article19. Absah I, Bruining DH, Matsumoto JM, Weisbrod AJ, Fletcher JG, Fidler JL, et al. MR enterography in pediatric inflammatory bowel disease: retrospective assessment of patient tolerance, image quality, and initial performance estimates. AJR Am J Roentgenol. 2012; 199:W367–W375.
Article20. Mollard BJ, Smith EA, Lai ME, Phan T, Christensen RE, Dillman JR. MR enterography under the age of 10 years: a single institutional experience. Pediatr Radiol. 2015; [Epub ahead of print].21. Mollard BJ, Smith EA, Dillman JR. Pediatric MR enterography: technique and approach to interpretation-how we do it. Radiology. 2015; 274:29–43.
Article22. Towbin AJ, Sullivan J, Denson LA, Wallihan DB, Podberesky DJ. CT and MR enterography in children and adolescents with inflammatory bowel disease. Radiographics. 2013; 33:1843–1860.
Article23. Anupindi SA, Terreblanche O, Courtier J. Magnetic resonance enterography: inflammatory bowel disease and beyond. Magn Reson Imaging Clin N Am. 2013; 21:731–750.24. Darge K, Anupindi SA, Jaramillo D. MR imaging of the abdomen and pelvis in infants, children, and adolescents. Radiology. 2011; 261:12–29.
Article25. Sinha R, Rajiah P, Murphy P, Hawker P, Sanders S. Utility of high-resolution MR imaging in demonstrating transmural pathologic changes in Crohn disease. Radiographics. 2009; 29:1847–1867.
Article26. Dillman JR, Smith EA, Khalatbari S, Strouse PJ. I.v. glucagon use in pediatric MR enterography: effect on image quality, length of examination, and patient tolerance. AJR Am J Roentgenol. 2013; 201:185–189.
Article27. Yacoub JH, Obara P, Oto A. Evolving role of MRI in Crohn's disease. J Magn Reson Imaging. 2013; 37:1277–1289.
Article28. Allen BC, Leyendecker JR. MR enterography for assessment and management of small bowel Crohn disease. Radiol Clin North Am. 2014; 52:799–810.
Article29. Fidler JL, Guimaraes L, Einstein DM. MR imaging of the small bowel. Radiographics. 2009; 29:1811–1825.
Article30. Masselli G, Gualdi G. MR imaging of the small bowel. Radiology. 2012; 264:333–348.
Article31. Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, Prassopoulos P. MR enteroclysis: technical considerations and clinical applications. Eur Radiol. 2002; 12:2651–2658.
Article32. Low RN, Sebrechts CP, Politoske DA, Bennett MT, Flores S, Snyder RJ, et al. Crohn disease with endoscopic correlation: single-shot fast spin-echo and gadolinium-enhanced fat-suppressed spoiled gradient-echo MR imaging. Radiology. 2002; 222:652–660.
Article33. Röttgen R, Grandke T, Grieser C, Lehmkuhl L, Hamm B, Ludemann L. Measurement of MRI enhancement kinetics for evaluation of inflammatory activity in Crohn's disease. Clin Imaging. 2010; 34:29–35.
Article34. Pupillo VA, Di Cesare E, Frieri G, Limbucci N, Tanga M, Masciocchi C. Assessment of inflammatory activity in Crohn's disease by means of dynamic contrast-enhanced MRI. Radiol Med. 2007; 112:798–809.
Article35. Sinha R, Rajiah P, Ramachandran I, Sanders S, Murphy PD. Diffusion-weighted MR imaging of the gastrointestinal tract: technique, indications, and imaging findings. Radiographics. 2013; 33:655–676. discussion 676-80
Article36. Kiryu S, Dodanuki K, Takao H, Watanabe M, Inoue Y, Takazoe M, et al. Free-breathing diffusion-weighted imaging for the assessment of inflammatory activity in Crohn's disease. J Magn Reson Imaging. 2009; 29:880–886.
Article37. Oto A, Zhu F, Kulkarni K, Karczmar GS, Turner JR, Rubin D. Evaluation of diffusion-weighted MR imaging for detection of bowel inflammation in patients with Crohn's disease. Acad Radiol. 2009; 16:597–603.
Article38. Maglinte DD, Gourtsoyiannis N, Rex D, Howard TJ, Kelvin FM. Classification of small bowel Crohn's subtypes based on multimodality imaging. Radiol Clin North Am. 2003; 41:285–303.
Article39. Zappa M, Stefanescu C, Cazals-Hatem D, Bretagnol F, Deschamps L, Attar A, et al. Which magnetic resonance imaging findings accurately evaluate inflammation in small bowel Crohn's disease? A retrospective comparison with surgical pathologic analysis. Inflamm Bowel Dis. 2011; 17:984–993.
Article40. Adler J, Punglia DR, Dillman JR, Polydorides AD, Dave M, Al-Hawary MM, et al. Computed tomography enterography findings correlate with tissue inflammation, not fibrosis in resected small bowel Crohn's disease. Inflamm Bowel Dis. 2012; 18:849–856.
Article41. Gee MS, Nimkin K, Hsu M, Israel EJ, Biller JA, Katz AJ, et al. Prospective evaluation of MR enterography as the primary imaging modality for pediatric Crohn disease assessment. AJR Am J Roentgenol. 2011; 197:224–231.
Article42. Rimola J, Rodriguez S, Garcia-Bosch O, Ordás I, Ayala E, Aceituno M, et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn's disease. Gut. 2009; 58:1113–1120.
Article43. Punwani S, Rodriguez-Justo M, Bainbridge A, Greenhalgh R, De Vita E, Bloom S, et al. Mural inflammation in Crohn disease: location-matched histologic validation of MR imaging features. Radiology. 2009; 252:712–720.
Article44. Sempere GA, Martinez Sanjuan V, Medina Chulia E, Benages A, Tome Toyosato A, Canelles P, et al. MRI evaluation of inflammatory activity in Crohn's disease. AJR Am J Roentgenol. 2005; 184:1829–1835.
Article45. Oto A, Kayhan A, Williams JT, Fan X, Yun L, Arkani S, et al. Active Crohn's disease in the small bowel: evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging. 2011; 33:615–624.
Article46. Koh DM, Miao Y, Chinn RJ, Amin Z, Zeegen R, Westaby D, et al. MR imaging evaluation of the activity of Crohn's disease. AJR Am J Roentgenol. 2001; 177:1325–1332.
Article47. Gourtsoyianni S, Papanikolaou N, Amanakis E, Bourikas L, Roussomoustakaki M, Grammatikakis J, et al. Crohn's disease lymphadenopathy: MR imaging findings. Eur J Radiol. 2009; 69:425–428.
Article48. Pariente B, Cosnes J, Danese S, Sandborn WJ, Lewin M, Fletcher JG, et al. Development of the Crohn's disease digestive damage score, the Lémann score. Inflamm Bowel Dis. 2011; 17:1415–1422.
Article49. Sinha R, Verma R, Verma S, Rajesh A. MR enterography of Crohn disease: part 2, imaging and pathologic findings. AJR Am J Roentgenol. 2011; 197:80–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed Tomography Enterography and Magnetic Resonance Enterography in the Diagnosis of Crohn's Disease
- Role of Computed Tomography Enterography/Magnetic Resonance Enterography: Is It in Prime Time?
- Preparation, Technique, and Imaging of Computed Tomography/Magnetic Resonance Enterography
- A Look into the Small Bowel in Crohn's Disease
- Magnetic resonance enterography for the evaluation of the deep small intestine in Crohn's disease