Long-Term Mortality According to the Characteristics of Early Neurological Deterioration in Ischemic Stroke Patients
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea. jhheo@yuhs.ac
- 2Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2068676
- DOI: http://doi.org/10.3349/ymj.2014.55.3.669
Abstract
- PURPOSE
Although early neurological deterioration (END) during the acute stroke period is known to be associated with poor functional outcomes, there is little data regarding the impact of END on long-term outcomes according to the characteristics of END. The aim of this study was to investigate whether there are differences in long-term mortality according to the characteristics of END among acute ischemic stroke or transient ischemic attack patients.
MATERIALS AND METHODS
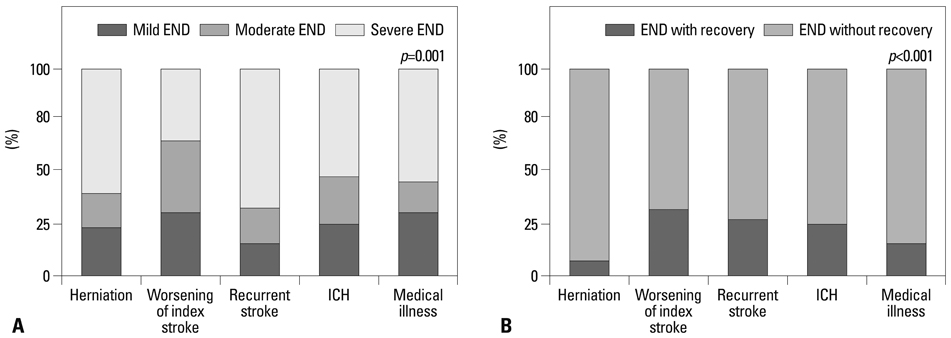
END was defined as any increase (> or =1) in National Institute of Health Stroke Scale score within 7 days after admission. We assessed the characteristics of END, such as the etiology and severity of END, as well as recovery after END. The relationship between 30-day or long-term mortality and each characteristic of END was investigated using multiple logistic analysis or Cox regression model.
RESULTS
Among 2820 patients, END was observed in 344 patients (12.2%). After adjustment for age, sex, underlying cardiovascular diseases, stroke severity, and stroke subtypes, END was associated with long-term mortality, whether it was mild or severe and whether or not it was followed by recovery. However, 30-day mortality was strongly related to the severity of END or the absence of recovery after END. Among the causes of END, recurrent stroke and medical illness were related to 30-day mortality, as well as long-term mortality, while brain herniation and intracranial hemorrhagic complications were only associated with 30-day mortality.
CONCLUSION
The results of the present study demonstrated that END is associated with higher mortality and the effects of END on short-term and long-term mortality depend on END characteristics.
MeSH Terms
Figure
Cited by 4 articles
-
Total Cerebral Small-Vessel Disease Score is Associated with Mortality during Follow-Up after Acute Ischemic Stroke
Tae-Jin Song, Jinkwon Kim, Dongbeom Song, Joonsang Yoo, Hye Sun Lee, Yong-Jae Kim, Hyo Suk Nam, Ji Hoe Heo, Young Dae Kim
J Clin Neurol. 2017;13(2):187-195. doi: 10.3988/jcn.2017.13.2.187.High Dietary Glycemic Load is Associated with Poor Functional Outcome in Patients with Acute Cerebral Infarction
Tae-Jin Song, Yoonkyung Chang, Min-Young Chun, Chan-Young Lee, A-Ram Kim, Yuri Kim, Yong-Jae Kim
J Clin Neurol. 2018;14(2):165-173. doi: 10.3988/jcn.2018.14.2.165.Impact of Time Interval between Index Event and Stenting on Periprocedural Risk in Patients with Symptomatic Carotid Stenosis
Wonsuck Han, Gyojun Hwang, Sung Han Oh, Jong Joo Lee, Mi Kyung Kim, Bong Sub Chung, Jong Kook Rhim, Seung Hun Sheen, Taehyung Kim
J Korean Neurosurg Soc. 2020;63(5):598-606. doi: 10.3340/jkns.2020.0113.Adrenocorticotropic hormone and β-endorphin concentration as a prognostic factor in patients with subarachnoid hemorrhage due to aneurysmal rupture
Geo-seong Park, Ha-young Choi, Hyoung-gyu Jang, Jung-soo Park, Eun-jeong Koh, Jong-Myeong Lee
J Cerebrovasc Endovasc Neurosurg. 2022;24(2):113-120. doi: 10.7461/jcen.2021.E2021.08.003.
Reference
-
1. Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003; 2:43–53.
Article2. Appelros P, Nydevik I, Viitanen M. Poor outcome after first-ever stroke: predictors for death, dependency, and recurrent stroke within the first year. Stroke. 2003; 34:122–126.3. Vernino S, Brown RD Jr, Sejvar JJ, Sicks JD, Petty GW, O'Fallon WM. Cause-specific mortality after first cerebral infarction: a population-based study. Stroke. 2003; 34:1828–1832.
Article4. Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011; 42:1489–1494.5. Adams HP Jr, Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR, et al. Baseline NIH Stroke Scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology. 1999; 53:126–131.
Article6. Chang KC, Lee HC, Tseng MC, Huang YC. Three-year survival after first-ever ischemic stroke is predicted by initial stroke severity: a hospital-based study. Clin Neurol Neurosurg. 2010; 112:296–301.
Article7. Henriksson KM, Farahmand B, Johansson S, Asberg S, Terént A, Edvardsson N. Survival after stroke--the impact of CHADS2 score and atrial fibrillation. Int J Cardiol. 2010; 141:18–23.
Article8. Weimar C, Mieck T, Buchthal J, Ehrenfeld CE, Schmid E, Diener HC, et al. Neurologic worsening during the acute phase of ischemic stroke. Arch Neurol. 2005; 62:393–397.
Article9. Dávalos A, Cendra E, Teruel J, Martinez M, Genís D. Deteriorating ischemic stroke: risk factors and prognosis. Neurology. 1990; 40:1865–1869.
Article10. DeGraba TJ, Hallenbeck JM, Pettigrew KD, Dutka AJ, Kelly BJ. Progression in acute stroke: value of the initial NIH stroke scale score on patient stratification in future trials. Stroke. 1999; 30:1208–1212.11. Sumer M, Ozdemir I, Erturk O. Progression in acute ischemic stroke: frequency, risk factors and prognosis. J Clin Neurosci. 2003; 10:177–180.
Article12. Birschel P, Ellul J, Barer D. Progressing stroke: towards an internationally agreed definition. Cerebrovasc Dis. 2004; 17:242–252.
Article13. Dávalos A, Toni D, Iweins F, Lesaffre E, Bastianello S, Castillo J. Neurological deterioration in acute ischemic stroke: potential predictors and associated factors in the European cooperative acute stroke study (ECASS) I. Stroke. 1999; 30:2631–2636.14. Thanvi B, Treadwell S, Robinson T. Early neurological deterioration in acute ischaemic stroke: predictors, mechanisms and management. Postgrad Med J. 2008; 84:412–417.
Article15. Toni D, Fiorelli M, Gentile M, Bastianello S, Sacchetti ML, Argentino C, et al. Progressing neurological deficit secondary to acute ischemic stroke. A study on predictability, pathogenesis, and prognosis. Arch Neurol. 1995; 52:670–675.
Article16. Lee BI, Nam HS, Heo JH, Kim DI. Yonsei Stroke Team. Yonsei Stroke Registry. Analysis of 1,000 patients with acute cerebral infarctions. Cerebrovasc Dis. 2001; 12:145–151.17. Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006; 355:779–787.
Article18. Eriksson SE, Olsson JE. Survival and recurrent strokes in patients with different subtypes of stroke: a fourteen-year follow-up study. Cerebrovasc Dis. 2001; 12:171–180.
Article19. Johnston SC, Leira EC, Hansen MD, Adams HP Jr. Early recovery after cerebral ischemia risk of subsequent neurological deterioration. Ann Neurol. 2003; 54:439–444.
Article20. Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. Stroke. 2009; 40:2276–2293.
Article21. Silver FL, Norris JW, Lewis AJ, Hachinski VC. Early mortality following stroke: a prospective review. Stroke. 1984; 15:492–496.
Article22. Barber M, Langhorne P, Rumley A, Lowe GD, Stott DJ. D-dimer predicts early clinical progression in ischemic stroke: confirmation using routine clinical assays. Stroke. 2006; 37:1113–1115.
Article23. Devuyst G, Karapanayiotides T, Ruchat P, Pusztaszeri M, Lobrinus JA, Jonasson L, et al. Ultrasound measurement of the fibrous cap in symptomatic and asymptomatic atheromatous carotid plaques. Circulation. 2005; 111:2776–2782.
Article24. Kang DW, Kwon SU, Yoo SH, Kwon KY, Choi CG, Kim SJ, et al. Early recurrent ischemic lesions on diffusion-weighted imaging in symptomatic intracranial atherosclerosis. Arch Neurol. 2007; 64:50–54.
Article25. Hong HJ, Kim YD, Cha MJ, Kim J, Lee DH, Lee HS, et al. Early neurological outcomes according to CHADS2 score in stroke patients with non-valvular atrial fibrillation. Eur J Neurol. 2012; 19:284–290.
Article26. Kang DW, Latour LL, Chalela JA, Dambrosia JA, Warach S. Early and late recurrence of ischemic lesion on MRI: evidence for a prolonged stroke-prone state? Neurology. 2004; 63:2261–2265.
Article27. Bae HJ, Yoon DS, Lee J, Kim BK, Koo JS, Kwon O, et al. In-hospital medical complications and long-term mortality after ischemic stroke. Stroke. 2005; 36:2441–2445.
Article28. Ingeman A, Andersen G, Hundborg HH, Svendsen ML, Johnsen SP. In-hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke. 2011; 42:3214–3218.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Induced Hypertensive Therapy in an Acute Ischemic Stroke Patient with Early Neurological Deterioration
- Inhibition of LPA5 Activity Provides Long-Term Neuroprotection in Mice with Brain Ischemic Stroke
- Diagnosis of Cerebrovascular Disease
- Comparison of the Clinical Course of Ischemic Stroke Depending on the Stroke Subtypes
- Deterioration and Recurrence in Flight Passengers with Ischemic Stroke: An Evidence Based Case Report