J Korean Neurosurg Soc.
2012 Apr;51(4):222-226. 10.3340/jkns.2012.51.4.222.
Waffle-Cone Technique Using Solitaire AB Stent
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. smyoon@sch.ac.kr
- 2Department of Neurosurgery, Soonchunhyang University Gumi Hospital, Gumi, Korea.
- KMID: 2066915
- DOI: http://doi.org/10.3340/jkns.2012.51.4.222
Abstract
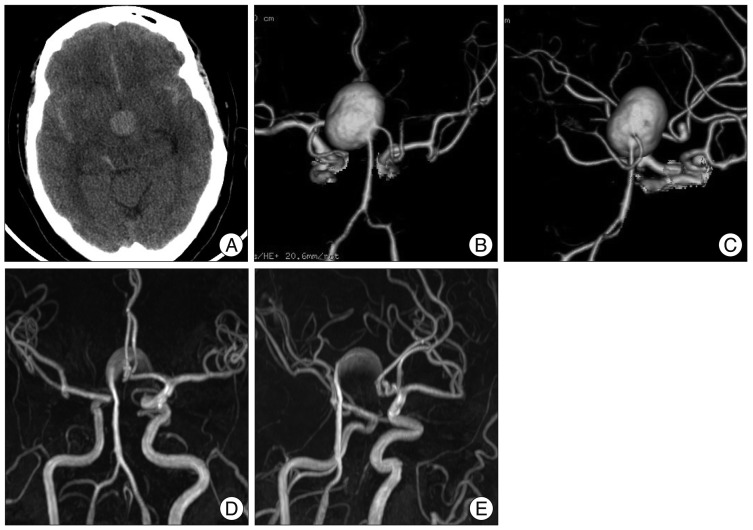
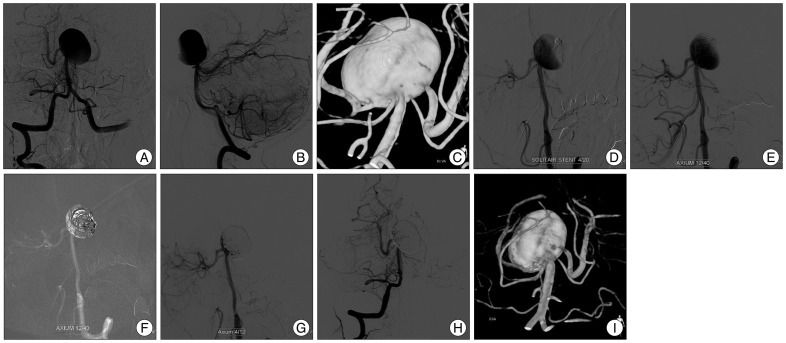
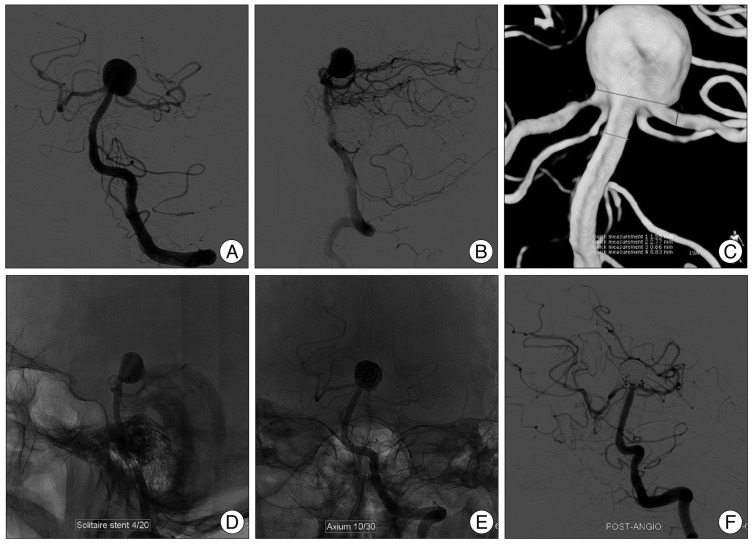
- The waffle-cone technique is a modified stent application technique, which involves protrusion of the distal portion of a stent into an aneurysm fundus to provide neck support for subsequent coiling. The authors report two cases of wide necked basilar bifurcation aneurysms, which were not amenable to stent assisted coiling, that were treated using the waffle-cone technique with a Solitaire AB stent. A 58-year-old woman presented with severe headache. Brain CT showed subarachnoid hemorrhage and angiography demonstrated a ruptured giant basilar bifurcation aneurysm with broad neck, which was treated with a Solitaire AB stent and coils using the waffle-cone technique. The second case involved an 81-year-old man, who presented with dizziness caused by brain stem infarction. Angiography also demonstrated a large basilar bifurcation unruptured aneurysm with broad neck. Solitaire AB stent deployment using the waffle-cone technique, followed by coiling resulted in near complete obliteration of aneurysm. The waffle-cone technique with a Solitaire AB stent can be a useful alternative to conventional stent application when it is difficult to catheterize bilateral posterior cerebral arteries in patients with a wide-necked basilar bifurcation aneurysm.
MeSH Terms
Figure
Cited by 2 articles
-
Iatrogenic Carotid-Cavernous Fistula after Stent Assisted Coil Embolization of Posterior Communicating Artery Aneurysm
Hye-Ran Park, Seok-Mann Yoon, Jai-Joon Shim, Hack-Gun Bae, Il-Gyu Yun
J Cerebrovasc Endovasc Neurosurg. 2015;17(1):43-48. doi: 10.7461/jcen.2015.17.1.43.Woven Endobridge (WEB) augmented by Y-stent in a shallow basilar tip aneurysm
Nathan J. Nordmann, Matthew W. Weber, Hayan Dayoub
J Cerebrovasc Endovasc Neurosurg. 2022;24(2):176-180. doi: 10.7461/jcen.2022.E2021.08.006.
Reference
-
1. Baldi S, Mounayer C, Piotin M, Spelle L, Moret J. Balloon-assisted coil placement in wide-neck bifurcation aneurysms by use of a new, compliant balloon microcatheter. AJNR Am J Neuroradiol. 2003; 24:1222–1225. PMID: 12812958.2. Biondi A, Janardhan V, Katz JM, Salvaggio K, Riina HA, Gobin YP. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms : strategies in stent deployment and midterm follow-up. Neurosurgery. 2007; 61:460–468. discussion 468-469. PMID: 17881956.3. Gruber DP, Crone KR. Endoscopic washout : a new technique for treating chronic subdural hematomas in infants. Pediatr Neurosurg. 1997; 27:292–295. PMID: 9655143.
Article4. Horikoshi T, Fukamachi A, Nishi H, Fukasawa I. Detection of intracranial aneurysms by three-dimensional time-of-flight magnetic resonance angiography. Neuroradiology. 1994; 36:203–207. PMID: 8041440.
Article5. Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms : eight cases using the waffle cone technique. Neurosurgery. 2006; 58:ONS-258–ONS-262. discussion ONS-262.6. Huang Q, Xu Y, Hong B, Zhao R, Zhao W, Liu J. Stent-assisted embolization of wide-neck anterior communicating artery aneurysms : review of 21 consecutive cases. AJNR Am J Neuroradiol. 2009; 30:1502–1506. PMID: 19461055.
Article7. Kelly ME, Turner RD 4th, Moskowitz SI, Gonugunta V, Hussain MS, Fiorella D. Delayed migration of a self-expanding intracranial microstent. AJNR Am J Neuroradiol. 2008; 29:1959–1960. PMID: 18719038.
Article8. Klisch J, Clajus C, Sychra V, Eger C, Strasilla C, Rosahl S, et al. Coil embolization of anterior circulation aneurysms supported by the Solitaire AB Neurovascular Remodeling Device. Neuroradiology. 2010; 52:349–359. PMID: 19644683.
Article9. Moret J, Cognard C, Weill A, Castaings L, Rey A. [Reconstruction technic in the treatment of wide-neck intracranial aneurysms. Long-term angiographic and clinical results. Apropos of 56 cases]. J Neuroradiol. 1997; 24:30–44. PMID: 9303942.10. Murao K, Yamada N, Miyamoto S, Hyuga T, Kudo T, Satow T. Identification of inflow zone of cerebral aneurysm by MRA for effective coil embolization. Surg Cereb Stroke. 2008; 36:459–463.
Article11. Perez-Arjona E, Fessler RD. Basilar artery to bilateral posterior cerebral artery 'Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms : report of three cases. Neurol Res. 2004; 26:276–281. PMID: 15142320.
Article12. Pierce DS, Rosero EB, Modrall JG, Adams-Huet B, Valentine RJ, Clagett GP, et al. Open-cell versus closed-cell stent design differences in blood flow velocities after carotid stenting. J Vasc Surg. 2009; 49:602–606. discussion 606. PMID: 19268763.
Article13. Ryu CW, Koh JS, Lee CY, Kim EJ. Endovascular management of the wide-neck aneurysms : the applications of the coils and catheter. Neurointervention. 2010; 5:71–78.
Article14. Sychra V, Klisch J, Werner M, Dettenborn C, Petrovitch A, Strasilla C, et al. Waffle-cone technique with Solitaire™ AB remodeling device : endovascular treatment of highly selected complex cerebral aneurysms. Neuroradiology. 2011; 53:961–972. PMID: 20821314.
Article15. Wanke I, Doerfler A, Schoch B, Stolke D, Forsting M. Treatment of wide-necked intracranial aneurysms with a self-expanding stent system : initial clinical experience. AJNR Am J Neuroradiol. 2003; 24:1192–1199. PMID: 12812954.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Modified 'Y-Configured Stents with Waffle Cone Technique' for Broad Neck Basilar Top Aneurysm
- Solitaire AB Stent-Assisted Coiling of Wide-Neck Micro Aneurysms
- Effectiveness and Technical Considerations of Solitaire Platinum 4×40 mm Stent Retriever in Mechanical Thrombectomy with Solumbra Technique
- Novel Noncrossing Y-Stent Technique Using Tapered Proximal End of a Solitaire AB Stent for Coil Embolization of Wide-Neck Bifurcation Aneurysms
- Outcomes of Stent-assisted Coil Embolization of Wide-necked Intracranial Aneurysms Using the Solitaire(TM) AB Neurovascular Remodeling Device