Obstet Gynecol Sci.
2015 Sep;58(5):377-384. 10.5468/ogs.2015.58.5.377.
Learning curve analysis of laparoscopic radical hysterectomy for gynecologic oncologists without open counterpart experience
- Affiliations
-
- 1Gynecologic Cancer Center, Ajou University School of Medicine, Suwon, Korea. drchang@ajou.ac.kr
- 2Department of Obstetrics and Gynecology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2058461
- DOI: http://doi.org/10.5468/ogs.2015.58.5.377
Abstract
OBJECTIVE
To evaluate the learning curve of laparoscopic radical hysterectomy (LRH) for gynecologic oncologists who underwent residency- and fellowship-training on laparoscopic surgery without previous experience in performing abdominal radical hysterectomy (ARH).
METHODS
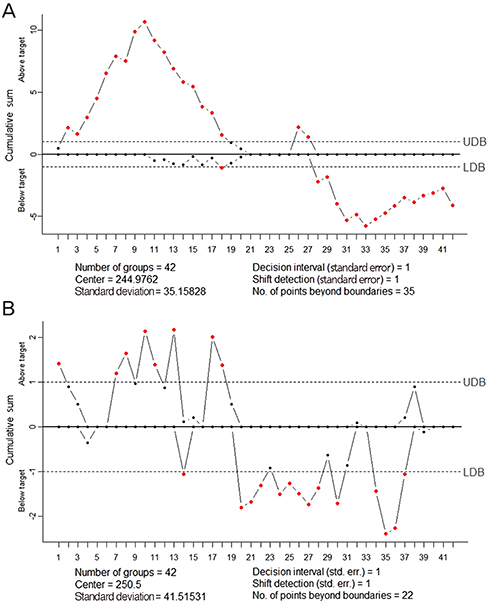
We retrospectively reviewed 84 patients with FIGO (International Federation of Gynecology and Obstetrics) stage IB cervical cancer who underwent LRH (Piver type III) between April 2006 and March 2014. The patients were divided into two groups (surgeon A group, 42 patients; surgeon B group, 42 patients) according to the surgeon with or without ARH experience. Clinico-pathologic data were analyzed between the 2 groups. Operating times were analyzed using the cumulative sum technique.
RESULTS
The operating time in surgeon A started at 5 to 10 standard deviations of mean operating time and afterward steeply decreased with operative experience (Pearson correlation coefficient=-0.508, P=0.001). Surgeon B, however, showed a gentle slope of learning curve within 2 standard deviations of mean operating time (Pearson correlation coefficient=-0.225, P=0.152). Approximately 18 cases for both surgeons were required to achieve surgical proficiency for LRH. Multivariate analysis showed that tumor size (>4 cm) was significantly associated with increased operating time (P=0.027; odds ratio, 4.667; 95% confidence interval, 1.187 to 18.352).
CONCLUSION
After completing the residency- and fellowship-training course on gynecologic laparoscopy, gynecologic oncologists, even without ARH experience, might reach an acceptable level of surgical proficiency in LRH after approximately 20 cases and showed a gentle slope of learning curve, taking less effort to initially perform LRH.
MeSH Terms
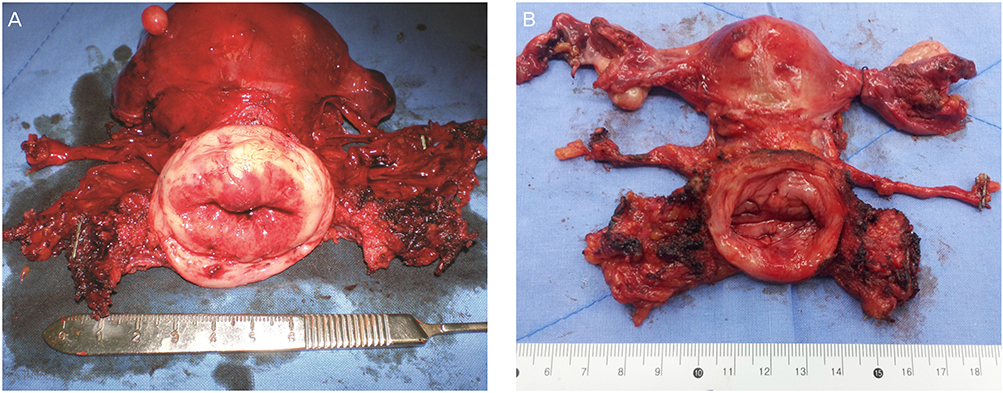
Figure
Cited by 1 articles
-
The comparison of surgical outcomes and learning curves of radical hysterectomy by laparoscopy and robotic system for cervical cancer: an experience of a single surgeon
Yoon Jung Heo, Seongmin Kim, Kyung Jin Min, Sanghoon Lee, Jin Hwa Hong, Jae Kwan Lee, Nak Woo Lee, Jae Yun Song
Obstet Gynecol Sci. 2018;61(4):468-476. doi: 10.5468/ogs.2018.61.4.468.
Reference
-
1. Pomel C, Atallah D, Le Bouedec G, Rouzier R, Morice P, Castaigne D, et al. Laparoscopic radical hysterectomy for invasive cervical cancer: 8-year experience of a pilot study. Gynecol Oncol. 2003; 91:534–539.2. Puntambekar SP, Palep RJ, Puntambekar SS, Wagh GN, Patil AM, Rayate NV, et al. Laparoscopic total radical hysterectomy by the Pune technique: our experience of 248 cases. J Minim Invasive Gynecol. 2007; 14:682–689.3. Nam JH, Park JY, Kim DY, Kim JH, Kim YM, Kim YT. Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol. 2012; 23:903–911.4. Choi CH, Lee JW, Lee YY, Kim HJ, Song T, Kim MK, et al. Comparison of laparoscopic-assisted radical vaginal hysterectomy and laparoscopic radical hysterectomy in the treatment of cervical cancer. Ann Surg Oncol. 2012; 19:3839–3848.5. Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008; 109:86–91.6. Cantrell LA, Mendivil A, Gehrig PA, Boggess JF. Survival outcomes for women undergoing type III robotic radical hysterectomy for cervical cancer: a 3-year experience. Gynecol Oncol. 2010; 117:260–265.7. Sert MB, Abeler V. Robot-assisted laparoscopic radical hysterectomy: comparison with total laparoscopic hysterectomy and abdominal radical hysterectomy; one surgeon's experience at the Norwegian Radium Hospital. Gynecol Oncol. 2011; 121:600–604.8. Tinelli R, Malzoni M, Cosentino F, Perone C, Fusco A, Cicinelli E, et al. Robotics versus laparoscopic radical hysterectomy with lymphadenectomy in patients with early cervical cancer: a multicenter study. Ann Surg Oncol. 2011; 18:2622–2628.9. Vickers AJ, Savage CJ, Hruza M, Tuerk I, Koenig P, Martinez-Pineiro L, et al. The surgical learning curve for laparoscopic radical prostatectomy: a retrospective cohort study. Lancet Oncol. 2009; 10:475–480.10. Reade C, Hauspy J, Schmuck ML, Moens F. Characterizing the learning curve for laparoscopic radical hysterectomy: buddy operating as a technique for accelerating skill acquisition. Int J Gynecol Cancer. 2011; 21:930–935.11. Hwang JH, Yoo HJ, Joo J, Kim S, Lim MC, Song YJ, et al. Learning curve analysis of laparoscopic radical hysterectomy and lymph node dissection in early cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2012; 163:219–223.12. Stolzenburg JU, Rabenalt R, Do M, Horn LC, Liatsikos EN. Modular training for residents with no prior experience with open pelvic surgery in endoscopic extraperitoneal radical prostatectomy. Eur Urol. 2006; 49:491–498.13. Williams SM, Parry BR, Schlup MM. Quality control: an application of the cusum. BMJ. 1992; 304:1359–1361.14. Bae JW, Lee JH, Choi JS, Son CE, Jeon SW, Hong JH, et al. Laparoscopic lymphadenectomy for gynecologic malignancies: evaluation of the surgical approach and outcomes over a seven-year experience. Arch Gynecol Obstet. 2012; 285:823–829.15. Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011; 25:855–860.16. Steed H, Rosen B, Murphy J, Laframboise S, De Petrillo D, Covens A. A comparison of laparascopic-assisted radical vaginal hysterectomy and radical abdominal hysterectomy in the treatment of cervical cancer. Gynecol Oncol. 2004; 93:588–593.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- Learning Curve and Clinicopathologic Analysis in Transperitoneal Laparoscopic Adrenalectomy; Performed by a Single Young Surgeon with No Experience of Open Adrenalectomy
- Learning curve analysis of robot-assisted radical hysterectomy for cervical cancer: initial experience at a single institution
- Transvaginal cervical tumor-concealing no-look no-touch technique in minimally invasive radical hysterectomy for early-stage cervical cancer: a novel operation technique
- Laparoscopic Assisted Vaginal Hysterectomy: A Review of 500 Cases