Hip Pelvis.
2014 Mar;26(1):55-61. 10.5371/hp.2014.26.1.55.
Uremic Tumoral Calcinosis around the Hip Joint in a Patient on Hemodialysis
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University College of Medicine, Seoul, Korea. knee@schmc.ac.kr
- KMID: 2054164
- DOI: http://doi.org/10.5371/hp.2014.26.1.55
Abstract
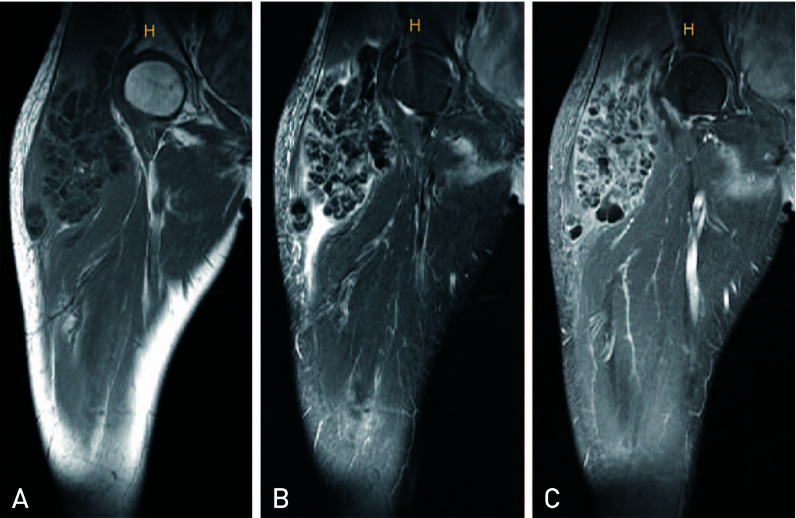
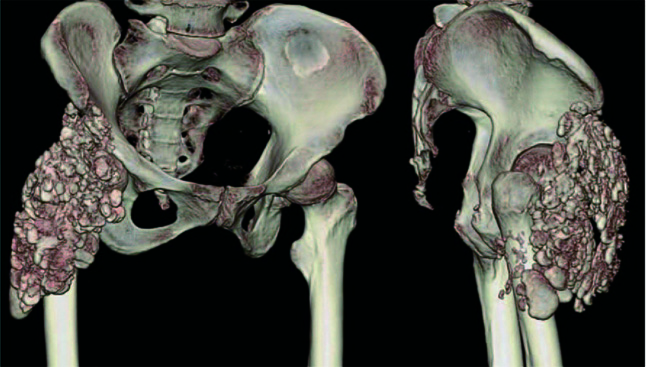
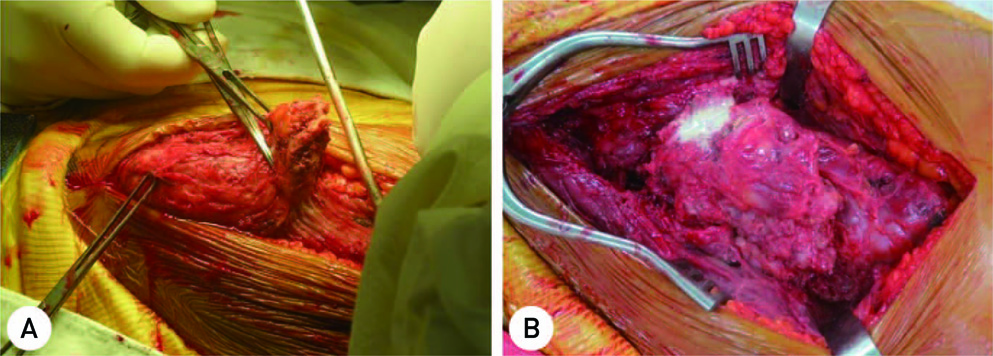
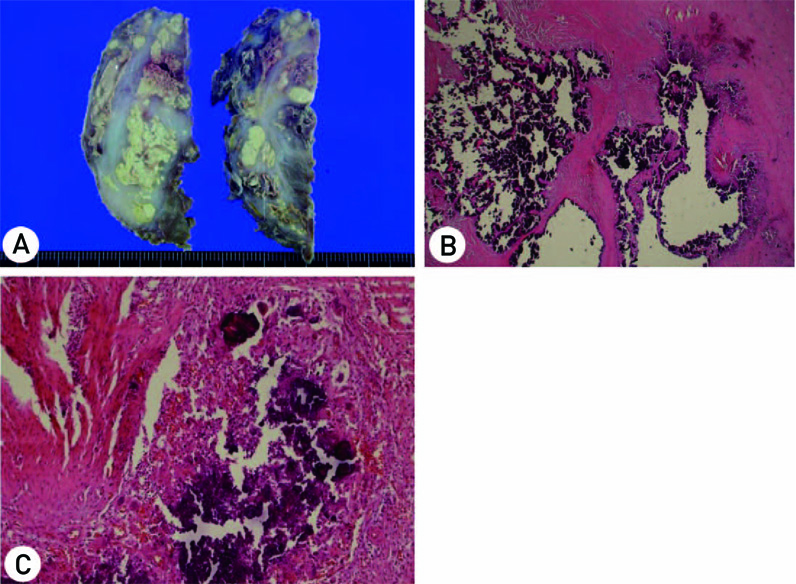
- The term tumoral calcinosis in used to describe the deposition of nodular calcareous masses in the soft tissue around large joints, such as the hips, shoulders, and elbows. Although the cause has not yet been clearly determined, according to the hypothesis, failure of phosphorus metabolism in the proximal tubule in kidney, chronic renal disease and hyperparathyroidism may cause tumoral calcinosis. No cases of tumoral calcinosis treated with surgical resection in chronic renal failure patients on hemodialysis, so called uremic tumoral calcinosis, have been reported in Korea. The authors experienced the case of a 57-year-old woman with chronic kidney disease on hemodialysis who presented with a mass around the hip. We made a diagnosis using plain radiographs, magnetic resonance imaging, and computed tomography of tumoral calcinosis, and treated the patient successfully with surgical resection. We report on a case of uremic tumoral calcinosis with a review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Inclan A, Leon P, Camejo MG. Tumoral Calcinosis. JAMA. 1943; 121:490–495.
Article2. Smit GG, Schmaman A. Tumoral calcinosis. J Bone Joint Surg Br. 1967; 49:698–703.
Article3. Mitnick PD, Goldfarb S, Slatopolsky E, Lemann J Jr, Gray RW, Agus ZS. Calcium and phosphate metabolism in tumoral calcinosis. Ann Intern Med. 1980; 92:482–487.
Article4. Chalmers GW, Brown WR, Stienstra JJ. Tumoral calcinosis-like lesion of the foot. A case report. J Am Podiatr Med Assoc. 1998; 88:87–91.
Article5. Prahinski JR, Schaefer RA. Tumoral calcinosis of the foot. Foot Ankle Int. 2001; 22:911–913.
Article6. Duret MH. Tumeurs multiples et singulieres des bourse sereuses. Bull Soc Anat Paris. 1899; 74:725–731.7. Teutschlaender O. Lipid calcinosis. Zieglers Beitr. 1947; 110:402–405.8. Martinez S, Vogler JB 3rd, Harrelson JM, Lyles KW. Imaging of tumoral calcinosis: new observations. Radiology. 1990; 174:215–222.
Article9. Smack D, Norton SA, Fitzpatrick JE. Proposal for a pathogenesis-based classification of tumoral calcinosis. Int J Dermatol. 1996; 35:265–271.
Article10. Olsen KM, Chew FS. Tumoral calcinosis: pearls, polemics, and alternative possibilities. Radiographics. 2006; 26:871–885.
Article11. Eisenberg B, Tzamaloukas AH, Hartshorne MF, Listrom MB, Arrington ER, Sherrard DJ. Periarticular tumoral calcinosis and hypercalcemia in a hemodialysis patient without hyperparathyroidism: a case report. J Nucl Med. 1990; 31:1099–1103.12. Zins B, Zingraff J, Basile C, et al. Tumoral calcifications in hemodialysis patients: possible role of aluminum intoxication. Nephron. 1992; 60:260–267.
Article13. Benkert A, Tschammler A, Bahner U, Heidbreder E, Hahn D. The follow-up assessment of tumorous calcinosis before and after parathyroidectomy in secondary hyperparathyroidism. Rofo. 1994; 161:90–92.
Article14. Thomason AJS, Frewer JD, Marya SK. Accessory patella. An unusual presentation of tumoral calcinosis. Orthopaedics. 1996; 4:207–208.15. Yeh SM, Hwang SJ, Chen HC. Treatment of severe metastatic calcification in hemodialysis patients. Hemodial Int. 2009; 13:163–167.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Resolution of uremic tumoral calcinosis in a patient on peritoneal dialysis with long-term low-calcium dialysate treatment
- Pathologic Fracture of Femoral Neck in a Patient with Tumoral Calcinosis
- Tumoral Calcinosis Around the Knee Joint: A Case Report
- A Case of Tumoral Calcinosis at the Auricle
- Tumoral Calcinosis of the Foot: MRI & Histologic Findings; Two Cases Report