Hip Pelvis.
2013 Jun;25(2):102-109. 10.5371/hp.2013.25.2.102.
The Usefulness of Intraoperative Radiography for Prevention of Malalignment of the Cemented Femoral Stem
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Veterans Hospital, Seoul, Korea. 3188yun@naver.com
- KMID: 2054146
- DOI: http://doi.org/10.5371/hp.2013.25.2.102
Abstract
- PURPOSE
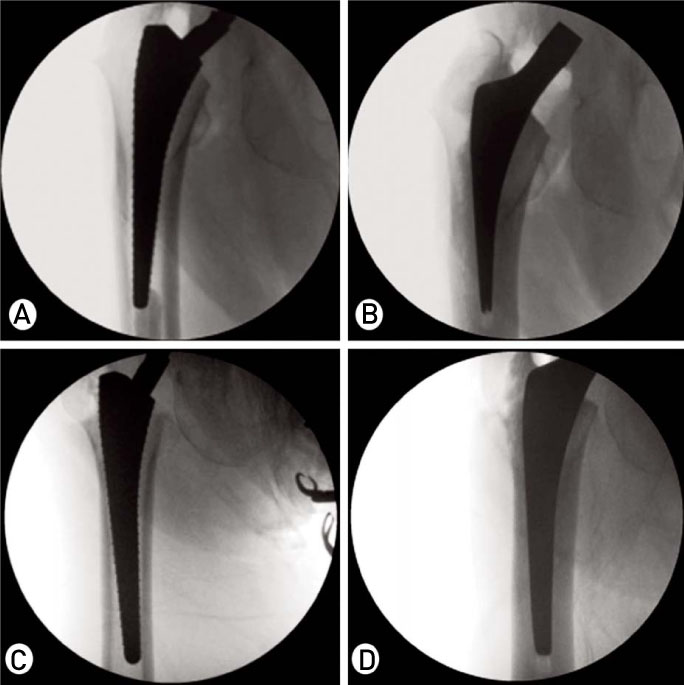
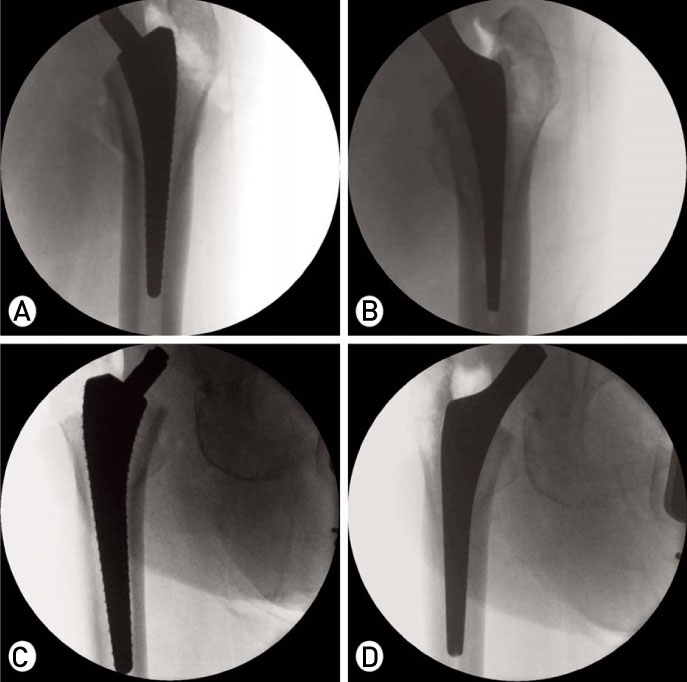
The purpose of this study was to evaluate the usefulness of our method, which estimated femoral stem alignment using a c-arm when the broach was inserted, for prevention of femoral stem malalignment.
MATERIALS AND METHODS
A total of 103 hips were enrolled in this study. All patients underwentprimary hip arthroplasty from October 2011 to February 2013. The study was conductedretrospectively. Intraoperative estimated femoral stem alignments and final femoral stem alignments were classified into three groups. Multinomial logistic regression analysis was performed for analysis of factors (age, sex, diagnosis, body mass index, femoral stem size, osteoporosis, and proximal demur geometry) thatmight affect intraoperatively estimated femoral stem alignment.
RESULTS
The distribution of intraoperative estimated femoral stem alignment was 80(78%) in the neutral group, 18(17%) in the varus group, and 5(5%) in the valgus group. The distribution of final femoral stem alignment was 100(97%) in the neutral group, 2(2%) in the varus group, and 1(1%) in the valgus group. There was no statistically significant factor affecting the intraoperatively estimated femoral stem alignment.
CONCLUSION
Intraoperative estimated femoral stem alignment using a c-arm is an effective method for prevention of femoral stem malalignment.
Keyword
Figure
Reference
-
1. Kitada M, Nakamura N, Iwana D, Kakimoto A, Nishii T, Sugano N. Evaluation of the accuracy of computed tomography-based navigation for femoral stem orientation and leg length discrepancy. J Arthroplasty. 2011; 26:674–679.
Article2. Herrlin K, Pettersson H, Selvik G, Lidgren L. Femoral anteversion and restricted range of motion in total hip prostheses. Acta Radiol. 1988; 29:551–553.
Article3. Müller M, Crucius D, Perka C, Tohtz S. The association between the sagittal femoral stem alignment and the resulting femoral head centre in total hip arthroplasty. Int Orthop. 2011; 35:981–987.
Article4. Min BW, Song KS, Bae KC, Cho CH, Kang CH, Kim SY. The effect of stem alignment on results of total hip arthroplasty with a cementless tapered-wedge femoral component. J Arthroplasty. 2008; 23:418–423.
Article5. Patel AB, Wagle RR, Usrey MM, Thompson MT, Incavo SJ, Noble PC. Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty. 2010; 25:1275–1281.
Article6. Khalily C, Lester DK. Results of a tapered cementless femoral stem implanted in varus. J Arthroplasty. 2002; 17:463–466.
Article7. Vresilovic EJ, Hozack WJ, Rothman RH. Radiographic assessment of cementless femoral components. Correlation with intraoperative mechanical stability. J Arthroplasty. 1994; 9:137–141.8. Jaffe WL, Hawkins CA. Normalized and proportionalized cemented femoral stem survivorship at 15 years. J Arthroplasty. 1999; 14:708–713.
Article09. Munuera L, Garcia-Cimbrelo E. The femoral component in low-friction arthroplasty after ten years. Clin Orthop Relat Res. 1992; 163–175.
Article10. Davis ET, Gallie P, Macgroarty K, Waddell JP, Schemitsch E. The accuracy of image-free computer navigation in the placement of the femoral component of the Birmingham Hip Resurfacing: a cadaver study. J Bone Joint Surg Br. 2007; 89:557–560.11. Hananouchi T, Sugano N, Nakamura N, et al. Preoperative templating of femoral components on plain X-rays. Rotational evaluation with synthetic X-rays on ORTHODOC. Arch Orthop Trauma Surg. 2007; 127:381–385.
Article12. Miller RG. Osteoporosis in postmenopausal women. Therapy options across a wide range of risk for fracture. Geriatrics. 2006; 61:24–30.13. Hauschild O, Ghanem N, Oberst M, et al. Evaluation of Singh index for assessment of osteoporosis using digital radiography. Eur J Radiol. 2009; 71:152–158.
Article14. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242.
Article15. Reitman RD, Emerson R, Higgins L, Head W. Thirteen year results of total hip arthroplasty using a tapered titanium femoral component inserted without cement in patients with type C bone. J Arthroplasty. 2003; 18:116–121.
Article16. Mollan RA, Watters PH, Steele R, McClelland CJ. Failure of the femoral component in the Howse total hip arthroplasty. Clin Orthop Relat Res. 1984; 142–147.
Article17. Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymüller Alloclassic system. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 2003; 85-A:296–303.18. Schramm M, Keck F, Hohmann D, Pitto RP. Total hip arthroplasty using an uncemented femoral component with taper design: outcome at 10-year follow-up. Arch Orthop Trauma Surg. 2000; 120:407–412.
Article19. Devitt A, O'Sullivan T, Quinlan W. 16- to 25-year follow-up study of cemented arthroplasty of the hip in patients aged 50 years or younger. J Arthroplasty. 1997; 12:479–489.
Article20. Munuera L, Garcia-Cimbrelo E. The femoral component in low-friction arthroplasty after ten years. Clin Orthop Relat Res. 1992; 163–175.
Article21. Macpherson GJ, Hank C, Schneider M, et al. The posterior approach reduces the risk of thin cement mantles with a straight femoral stem design. Acta Orthop. 2010; 81:292–295.
Article22. Ebramzadeh E, Sarmiento A, McKellop HA, Llinas A, Gogan W. The cement mantle in total hip arthroplasty. Analysis of long-term radiographic results. J Bone Joint Surg Am. 1994; 76:77–87.
Article23. Joshi RP, Eftekhar NS, McMahon DJ, Nercessian OA. Osteolysis after Charnley primary low-friction arthroplasty. A comparison of two matched paired groups. J Bone Joint Surg Br. 1998; 80:585–590.24. Smith SW, Estok DM 2nd, Harris WH. Total hip arthroplasty with use of second-generation cementing techniques. An eighteen-year-average follow-up study. J Bone Joint Surg Am. 1998; 80:1632–1640.
Article25. Woolson ST, Milbauer JP, Bobyn JD, Yue S, Maloney WJ. Fatigue fracture of a forged cobalt-chromium-molybdenum femoral component inserted with cement. A report of ten cases. J Bone Joint Surg Am. 1997; 79:1842–1848.
Article26. Kawate K, Ohmura T, Hiyoshi N, Natsume Y, Teranishi T, Tamai S. Thin cement mantle and osteolysis with a precoated stem. Clin Orthop Relat Res. 1999; 124–129.
Article27. Mann KA, Gupta S, Race A, Miller MA, Cleary RJ, Ayers DC. Cement microcracks in thin-mantle regions after in vitro fatigue loading. J Arthroplasty. 2004; 19:605–612.
Article28. Ramos A, Simões JA. The influence of cement mantle thickness and stem geometry on fatigue damage in two different cemented hip femoral prostheses. J Biomech. 2009; 42:2602–2610.
Article29. Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992; 74:385–389.
Article30. Yi JW, Shon WY, Huh CH, Yun HH, Huh YJ. Follow-up study of the cemented polished femoral stem for more than five years. J Korean Hip Soc. 2011; 23:25–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Follow-up Results of Femoral Revision Hip Arthroplasty Using Impaction Bone Grafting and Standard Cemented Polished Stem
- Ceramic-on-Ceramic Bearing Total Hip Arthroplasty: Five-Year Midterm Follow-up Results
- Cemented Femoral Component with Centralizing Device : Is it Effective for Centralization and for Attainment of Optimal Cement Mantle Thickness ?
- Displacement of Polished Femoral Stem during Reduction of a Dislocated Cemented Total Hip Arthroplasty: A Case Report
- Results of Ceramic on Ceramic Bearing Total Hip Arthroplasty Using Cemented Femoral Stem and Cementless Femoral Stem