Hip Pelvis.
2012 Sep;24(3):213-221. 10.5371/hp.2012.24.3.213.
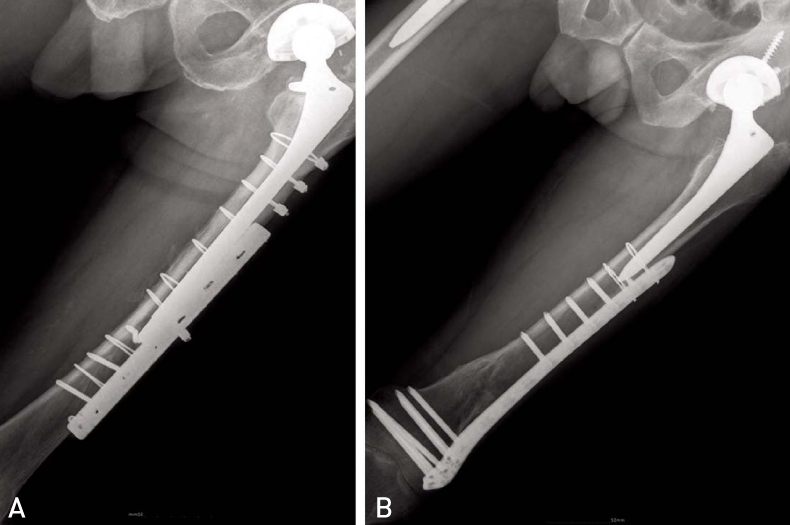
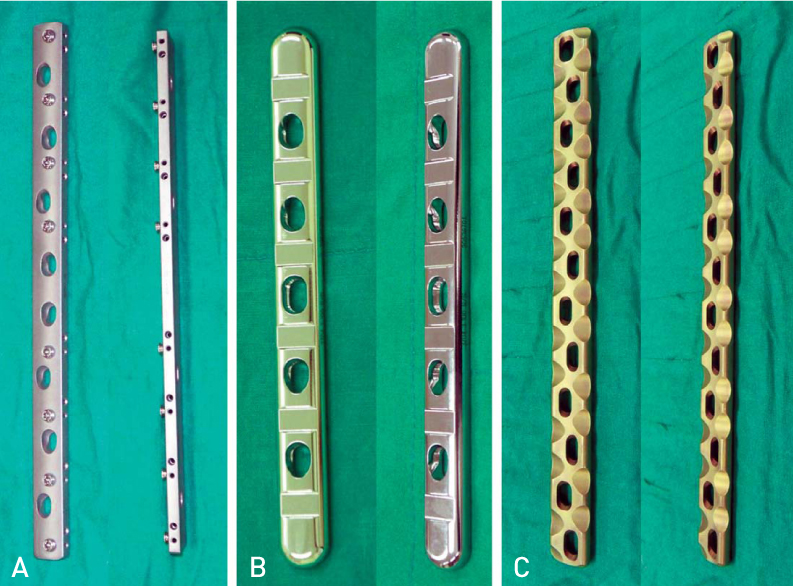
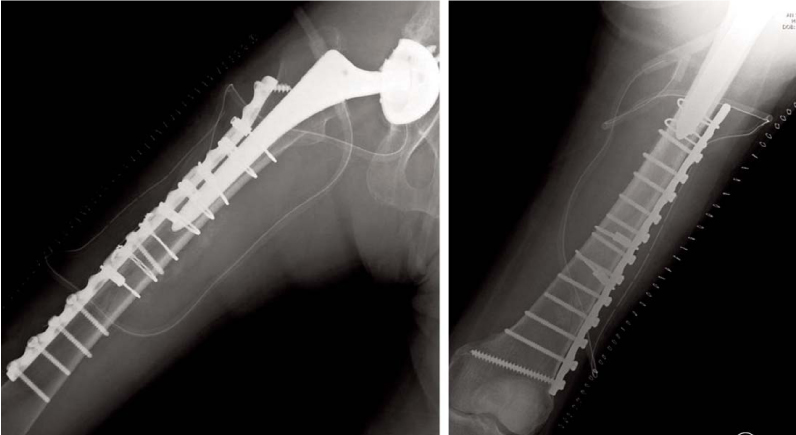
Operative Treatment of Periprosthetic Unstable Femoral Fractures of Vancouver Type B1 and C with Variable Plates
- Affiliations
-
- 1Department of Orthopedic Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. dreami3e5t@pusan.ac.kr
- KMID: 2054135
- DOI: http://doi.org/10.5371/hp.2012.24.3.213
Abstract
- PURPOSE
The purpose of this study is to evaluate the outcome after operative treatment with plate fixation in Vancouver B1 and C periprosthetic unstable femoral fractures.
MATERIALS AND METHODS
We conducted a retrospective assessment of 15 patients who had under gone treatment for a periprosthetic unstable femoral fracture around primary hip arthroplasty between April 1997 and July 2010. The mean age of patients was 69 years(53 to 82 years) at the time of surgery and the mean duration of follow-up was 29.2 months (six to 110 months). According to Vancouver classification, 10 patients were type B1 and five were type C. According to the time of operation, open reduction and internal fixation was performed using four different plates. Bone graft was applied in all patients, regardless of the type of plate. The present review describes the clinical and radiographic results.
RESULTS
All patients were able to ambulate without assistance of crutches or walkers. Of the 15 patients, the fracture site was united in all patients. Postoperative dislocation of the ipsilateral hip was observed in one patient; however, there was no occurrence of further complications, such as infections, nerve injuries, or loosening of the femoral stems.
CONCLUSION
In Vancouver type B1 and C fractures, without any loosening of the femoral stems, open reduction with plate fixation using our operative methods provided a satisfactory result.
MeSH Terms
Figure
Reference
-
1. Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005. 20:857–865.2. Laurer HL, Wutzler S, Possner S, et al. Outcome after operative treatment of Vancouver type B1 and C periprosthetic femoral fractures: open reduction and internal fixation versus revision arthroplasty. Arch Orthop Trauma Surg. 2011. 131:983–989.
Article3. Lewallen DG, Berry DJ. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect. 1998. 47:243–249.4. Bethea JA 3rd, DeAndrade JR, Fleming LL, Lindenbaum SD, Welch RB. Proximal femoral fractures following total hip arthroplasty. Clin Orthop Relat Res. 1982. (170):95–106.
Article5. Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course lect. 1995. 44:293–304.6. Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver Type B1 and Type C periprosthetic fractures of femur: a report on 12 patients. Injury. 2007. 38:725–733.
Article7. Beals RK, Tower SS. Periprosthetic fracture of the femur. An analysis of 93 fractures. Clin Orthop Relat Res. 1996. (327):238–246.8. Kim KS, Chung YY, Ryu SW, Choi CH, Jung HG. Management of ipsilateral femoral fracture after hip arthroplasty. J Korean Orthop Assoc. 1997. 32:1575–1583.
Article9. Ogden WS, Rendall J. Fractures beneath hip prosthesis: a special indication for parham bands and plating. Orthop Trans. 1978. 2:70.10. McElfresh EC, Coventry MB. Femoral and pelvic fractures after total hip arthroplasty. J Bone Joint Surg Am. 1974. 56:483–492.
Article11. Larsen E, Menck H, Rosenklint A. Fractures after hemialloplastic hip replacement. J Trauma. 1987. 27:72–74.
Article12. Lindahl H, Odén A, Garellick G, Malchau H. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007. 40:1294–1298.
Article13. Bhattacharyya T, Chang D, Meigs JB, Estok DM 2nd, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007. 89:2658–2662.
Article14. Johansson JE, McBroom R, Barrington TW, Hunter GA. Fracture of the ipsilateral femur in patients with total hip replacement. J Bone Joint Surg Am. 1981. 63:1435–1442.
Article15. McLauchlan GJ, Robinsson CM, Singer BR, Christie J. Results of an operative policy in the treatment of periprosthetic femoral fracture. J Orthop Trauma. 1997. 11:170–179.
Article16. Jensen JS, Barfod G, Hansen D, et al. Femoral shaft fracture after hip arthroplasty. Acta Orthop Scand. 1988. 59:9–13.
Article17. Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE. Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty. 2000. 15:523–528.
Article18. Schmotzer H, Tchejeyan GH, Dall DM. Surgical management of intra- and postoperative fractures of the femur about the tip of the stem in total hip arthroplasty. J Arthroplasty. 1996. 11:709–717.
Article19. Fulkerson E, Koval K, Preston CF, Iesaka K, Kummer FJ, Egol KA. Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plate. J Orthop Trauma. 2006. 20:89–93.
Article20. Larson JE, Chao EYS, Fitzgerald RH. Bypassing femoral cortical defects with cemented intramedullary stems. J Orthop Res. 1991. 9:414–421.
Article21. Hou Z, Moore B, Bowen TR, et al. Treatment of interprosthetic fractures of the femur. J Trauma. 2011. 71:1715–1719.
Article22. Wood GC, Naudie DR, Mcauley J, McCalden RW. Locking compression plates for the treatment of periprosthetic femoral fractures around well-fixed total hip and knee implants. J Arthroplasty. 2011. 26:886–892.
Article23. ElMaraghy AW, ElMaraghy MW, Nousiainen M, Richards RR, Schemitsch EH. Influence of the number of cortices on the stiffness of plate fixation of diaphyseal fractures. J Orthop Trauma. 2001. 15:186–191.
Article24. Cooke PH, Newman JH. Fractures of the femur in relation to cemented hip prostheses. J Bone Joint Surg Br. 1988. 70:386–389.
Article25. Serocki JH, Chandler RW, Dorr LD. Treatment of fractures about hip prostheses with compression plating. J Arthroplasty. 1992. 7:129–135.
Article26. Rüedi TP, Lüscher JN. Results after internal fixation of comminuted fractures of the femoral shaft with DC plates. Clin Orthop Relat Res. 1979. (138):74–76.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty
- Periprosthetic Femoral Fractures after Hip Arthroplasty
- Recurrent Treatment Failure in Vancouver Classification Type C Periprosthetic Fractures around a Well Fixed Short Femoral Stem
- Treatment of Periprosthetic Femoral Fractures with Cable Plate
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty