Pediatr Gastroenterol Hepatol Nutr.
2013 Sep;16(3):185-189. 10.5223/pghn.2013.16.3.185.
A Case of Esophageal Candidiasis in an Adolescent Who Had Frequently Received Budesonide Nebulizing Therapy
- Affiliations
-
- 1Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea. kyjoo@hanyang.ac.kr
- KMID: 2051332
- DOI: http://doi.org/10.5223/pghn.2013.16.3.185
Abstract
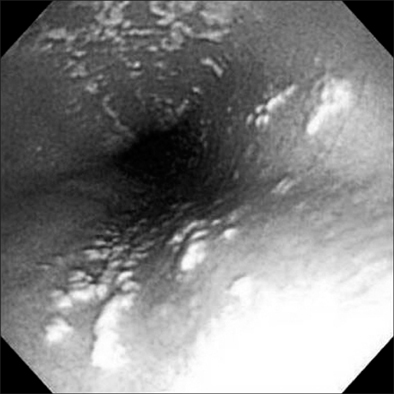
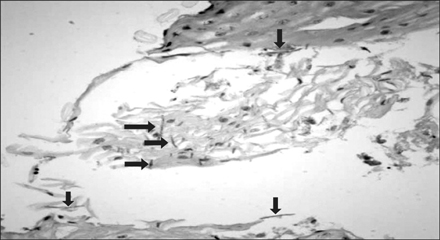
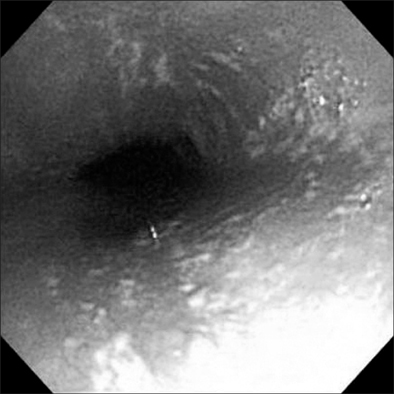
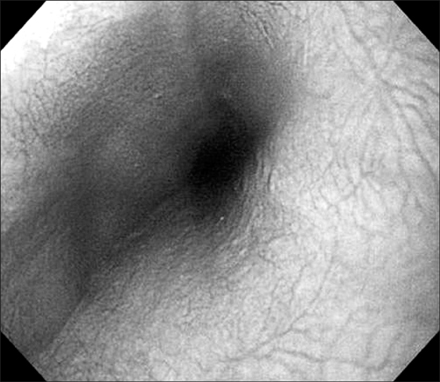
- Corticosteroid (budesonide) nebulizer therapy is commonly performed. Its side effects have been considered as being safe or ignorable. The authors present a case of esophageal candidiasis in a healthy female adolescent who was treated with budesonide nebulizer therapy a few times for a cough during the previous winter season. This child presented with dysphagia and epigastric pain for 1 month. Esophageal endoscopy showed a whitish creamy pseudomembrane and erosions on the esophageal mucosa. Pathologic findings showed numerous candidal hyphae. She did not show any evidence of immunodeficiency, clinically and historically. The esophageal lesion did not resolve naturally. The esophageal lesion completely improved with the antifungal therapy for 2 weeks; the symptoms disappeared, and the patient returned to normal health. It is important that frequent esophageal exposure to topical corticosteroids application can cause unexpected side effects.
Keyword
MeSH Terms
Figure
Reference
-
1. Mullaoglu S, Turktas H, Kokturk N, Tuncer C, Kalkanci A, Kustimur S. Esophageal candidiasis and Candida colonization in asthma patients on inhaled steroids. Allergy Asthma Proc. 2007; 28:544–549.
Article2. Aun MV, Ribeiro MR, Costa Garcia CL, Agondi RC, Kalil J, Giavina-Bianchi P. Esophageal candidiasis--an adverse effect of inhaled corticosteroids therapy. J Asthma. 2009; 46:399–401.
Article3. Vazquez JA. Optimal management of oropharyngeal and esophageal candidiasis in patients living with HIV infection. HIV AIDS (Auckl). 2010; 2:89–101.
Article4. Misra S, Ament ME. Esophagitis. In : Feigin RD, Cherry JD, editors. Textbook of pediatric infectious diseases. 4th ed. Philadelphia: Saunders;1997. p. 562–566.5. Kliemann DA, Pasqualotto AC, Falavigna M, Giaretta T, Severo LC. Candida esophagitis: species distribution and risk factors for infection. Rev Inst Med Trop Sao Paulo. 2008; 50:261–263.
Article6. Mathieson R, Dutta SK. Candida esophagitis. Dig Dis Sci. 1983; 28:365–370.
Article7. Kanda N, Yasuba H, Takahashi T, Mizuhara Y, Yamazaki S, Imada Y, et al. Prevalence of esophageal candidiasis among patients treated with inhaled fluticasone propionate. Am J Gastroenterol. 2003; 98:2146–2148.
Article8. Shuto H, Nagata M, Terashi Y, Yamaguchi M, Takizawa T, Shuto C, et al. Esophageal candidiasis as complication of inhaled steroid therapy. Arerugi. 2003; 52:1053–1064.9. Kim YJ, Jang SJ. Esophagus, stomach & intestine; a case of esophageal candidiasis presenting recurrent abdominal pain in an immunocompetent child. Korean J Gastrointest Endosc. 1997; 17:55–58.10. Hasosah MY, Showail M, Al-Sahafi A, Satti M, Jacobson K. Esophageal candidiasis in an immunocompetent girl. World J Pediatr. 2009; 5:152–154.
Article11. Ostrosky-Zeichner L, Rex JH, Bennett J, Kullberg BJ. Deeply invasive candidiasis. Infect Dis Clin North Am. 2002; 16:821–835.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of esophageal candidiasis caused by inhaled corticosteroid
- A Case of Esophageal Candidiasis in a Healthy Child
- Recurrent Esophageal Stricture Caused by Candidiasis in an HIV-Infected Patient
- Esophagus, Stomach & Intestine; A Case of Esophageal Candidiasis Presenting Recurrent Abdominal Pain in an Immunocompetent Child
- A Case of Aggravated Esophageal Candidiasis and Gastric Yeast Bezoar Formation following Gastric Outlet Obstruction due to Duodenal Stenosis