Clin Endosc.
2014 May;47(3):270-274. 10.5946/ce.2014.47.3.270.
Acute Duodenal Ischemia and Periampullary Intramural Hematoma after an Uneventful Endoscopic Retrograde Cholangiopancreatography in a Patient with Primary Myelofibrosis
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. sean4h@korea.ac.kr
- KMID: 2049026
- DOI: http://doi.org/10.5946/ce.2014.47.3.270
Abstract
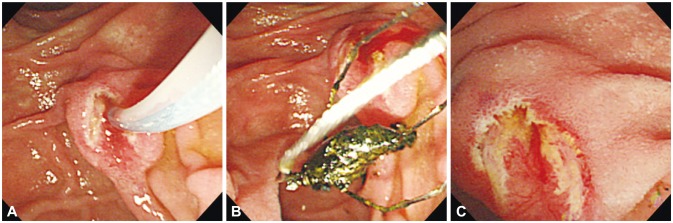
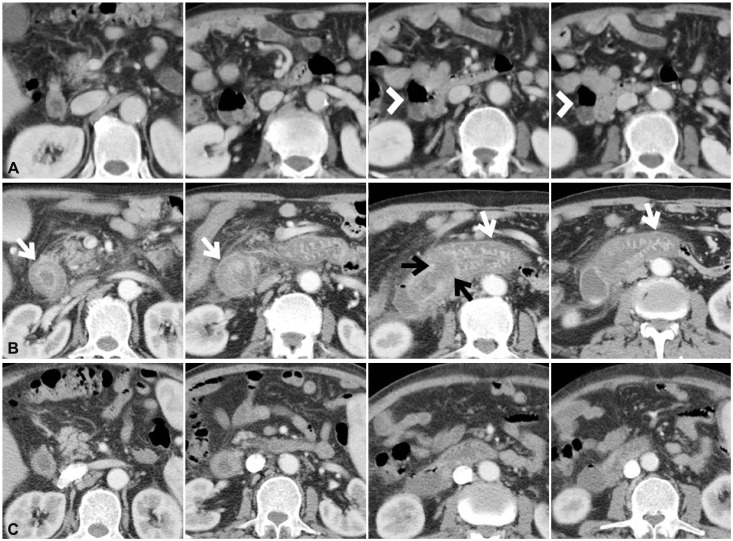
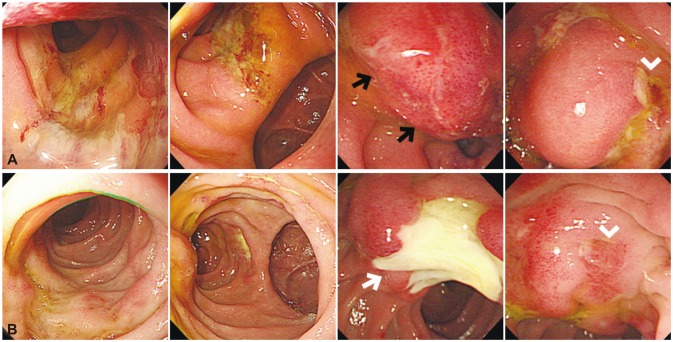
- Acute duodenal ischemia and periampullary intramural hematoma are rare complications after endoscopic retrograde cholangiopancreatography (ERCP). A 77-year-old man with splenomegaly complained of abdominal pain caused by common bile duct (CBD) stone. After successful removal of the CBD stone without immediate complications, the patient developed intramural hematoma around the ampulla of Vater along with diffuse duodenal edema. The findings were compatible with acute intestinal ischemia, and further evaluation revealed that he had underlying primary myelofibrosis. Myeloproliferative diseases are known to be significantly associated with an increased risk of thrombohemorrhagic complications. Therefore, particular attention should be given to this group of patients when a high-risk procedure such as ERCP is performed.
Keyword
MeSH Terms
Figure
Reference
-
1. Pannu HK, Fishman EK. Complications of endoscopic retrograde cholangiopancreatography: spectrum of abnormalities demonstrated with CT. Radiographics. 2001; 21:1441–1453. PMID: 11706215.
Article2. Barbui T, Finazzi G, Falanga A. Myeloproliferative neoplasms and thrombosis. Blood. 2013; 122:2176–2184. PMID: 23823316.
Article3. Melato M, Falconieri G, Manconi R, Bucconi S. Intramural gastric hematoma and hemoperitoneum occurring in a patient affected by idiopathic myelofibrosis. Hum Pathol. 1980; 11:301–302. PMID: 7399522.
Article4. Tefferi A. Primary myelofibrosis: 2013 update on diagnosis, risk-stratification, and management. Am J Hematol. 2013; 88:141–150. PMID: 23349007.
Article5. Tefferi A. Myelofibrosis with myeloid metaplasia. N Engl J Med. 2000; 342:1255–1265. PMID: 10781623.
Article6. Reilly JT, McMullin MF, Beer PA, et al. Guideline for the diagnosis and management of myelofibrosis. Br J Haematol. 2012; 158:453–471. PMID: 22651893.
Article7. Barbui T, Carobbio A, Cervantes F, et al. Thrombosis in primary myelofibrosis: incidence and risk factors. Blood. 2010; 115:778–782. PMID: 19965680.
Article8. Vannucchi AM. Management of myelofibrosis. Hematology Am Soc Hematol Educ Program. 2011; 2011:222–230. PMID: 22160038.9. Papadakis E, Hoffman R, Brenner B. Thrombohemorrhagic complications of myeloproliferative disorders. Blood Rev. 2010; 24:227–232. PMID: 20817333.
Article10. Leoni P, Rupoli S, Lai G, et al. Platelet abnormalities in idiopathic myelofibrosis: functional, biochemical and immunomorphological correlations. Haematologica. 1994; 79:29–39. PMID: 15378946.11. Finazzi G, Carobbio A, Thiele J, et al. Incidence and risk factors for bleeding in 1104 patients with essential thrombocythemia or prefibrotic myelofibrosis diagnosed according to the 2008 WHO criteria. Leukemia. 2012; 26:716–719. PMID: 21926959.
Article12. Diniz-Santos DR, de Andrade Cairo RC, Braga H, Araújo-Neto C, Paes IB, Silva LR. Duodenal hematoma following endoscopic duodenal biopsy: a case report and review of the existing literature. Can J Gastroenterol. 2006; 20:39–42. PMID: 16432559.13. Guzman C, Bousvaros A, Buonomo C, Nurko S. Intraduodenal hematoma complicating intestinal biopsy: case reports and review of the literature. Am J Gastroenterol. 1998; 93:2547–2550. PMID: 9860424.
Article14. ASGE Standards of Practice Committee. Anderson MA, Ben-Menachem T, et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc. 2009; 70:1060–1070. PMID: 19889407.
Article15. Bobadilla JL. Mesenteric ischemia. Surg Clin North Am. 2013; 93:925–940. PMID: 23885938.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramural Duodenal Hematoma after Transpancreatic Septotomy during ERCP: A Case Report and Literature Review
- The Management of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforation
- Four Cases of Guidewire Induced Periampullary Perforation During Endoscopic Retrograde Cholangiopancreatography
- Successful Endoscopic Decompression for Intramural Duodenal Hematoma with Gastric Outlet Obstruction Complicating Acute Pancreatitis
- A Case of Intramural Duodenal Hematoma after the Use of the Endoscopic Epinephrine Injection Method for Duodenal Ulcer Bleeding in a Chronic Renal Failure Patient undergoing Maintenance Hemodialysis