Clin Endosc.
2013 May;46(3):293-296. 10.5946/ce.2013.46.3.293.
A Case of Anisakiasis Invading the Stomach and the Colon at the Same Time after Eating Anchovies
- Affiliations
-
- 1Department of Internal Medicine, Daejeon Sun Hospital, Daejeon, Korea. 115203@naver.com
- KMID: 2048937
- DOI: http://doi.org/10.5946/ce.2013.46.3.293
Abstract
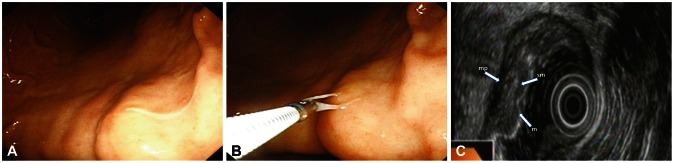
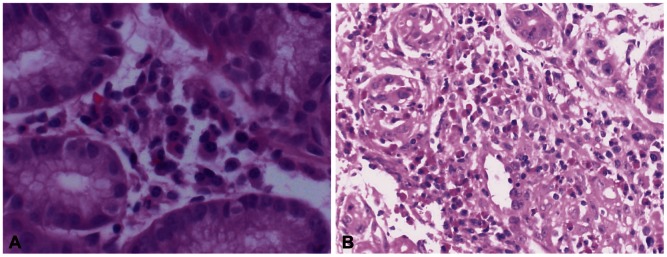
- Anisakiasis of the gastrointestinal tract is caused by the ingestion of raw fish or uncooked food infested with Anisakis larvae. A large number of cases of gastric anisakiasis have been reported in countries where the eating of raw fish is customary. However, there have been few reports of anisakiasis of the colon confirmed by colonoscopy and also very few reports of endoscopic ultrasonographic findings of anisakiasis. A 47-year-old man had epigastric pain with nausea after eating raw anchovies. Endoscopy found a living tubular structure penetrating into the lesser curvature of the stomach and the midtranseverse colon area. It was withdrawn with biopsy forceps. We report a case of anisakiasis simultaneously invading the stomach and the colon confirmed by endosopic utrasonographic findings and biopsy findings.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Status of common parasitic diseases in Korea in 2019
Sun Huh
J Korean Med Assoc. 2019;62(8):437-456. doi: 10.5124/jkma.2019.62.8.437.
Reference
-
1. Moreno-Ancillo A, Caballero MT, Cabañas R, et al. Allergic reactions to anisakis simplex parasitizing seafood. Ann Allergy Asthma Immunol. 1997; 79:246–250. PMID: 9305232.
Article2. Sakanari JA, McKerrow JH. Anisakiasis. Clin Microbiol Rev. 1989; 2:278–284. PMID: 2670191.
Article3. Kobayashi A, Tsuji M, Wilbur DL. Probable pulmonary anisakiasis accompanying pleural effusion. Am J Trop Med Hyg. 1985; 34:310–313. PMID: 3920926.4. Rushovich AM, Randall EL, Caprini JA, Westenfelder GO. Omental anisakiasis: a rare mimic of acute appendicitis. Am J Clin Pathol. 1983; 80:517–520. PMID: 6624718.
Article5. Yokogawa M, Yoshimura H. Clinicopathologic studies on larval anisakiasis in Japan. Am J Trop Med Hyg. 1967; 16:723–728. PMID: 6066221.
Article6. Sugimachi K, Inokuchi K, Ooiwa T, Fujino T, Ishii Y. Acute gastric anisakiasis. Analysis of 178 cases. JAMA. 1985; 253:1012–1013. PMID: 4038525.
Article7. Alonso-Gómez A, Moreno-Ancillo A, López-Serrano MC, et al. Anisakis simplex only provokes allergic symptoms when the worm parasitises the gastrointestinal tract. Parasitol Res. 2004; 93:378–384. PMID: 15221464.
Article8. Kim SG, Jo YJ, Park YS, et al. Four cases of gastric submucosal mass suspected as anisakiasis. Korean J Parasitol. 2006; 44:81–86. PMID: 16514287.
Article9. Yazaki Y, Namiki M. Biopsy of gastric anisakiasis with acute symptoms. In : Ishikawa H, Namiki M, editors. Gastric Anisakiasis in Japan. 1st ed. Tokyo: Springer-Verlag;1988. p. 113–116.10. Fujisawa K, Matsumoto T, Yoshimura R, Ayabe S, Tominaga M. Endoscopic finding of a large vanishing tumor. Endoscopy. 2001; 33:820. PMID: 11558039.
Article11. Muraoka A, Suehiro I, Fujii M, et al. Acute gastric anisakiasis: 28 cases during the last 10 years. Dig Dis Sci. 1996; 41:2362–2365. PMID: 9011443.12. Sakai K, Ohtani A, Muta H, et al. Endoscopic ultrasonography findings in acute gastric anisakiasis. Am J Gastroenterol. 1992; 87:1618–1623. PMID: 1442686.13. Okai T, Mouri I, Yamaguchi Y, Ohta H, Motoo Y, Sawabu N. Acute gastric anisakiasis: observations with endoscopic ultrasonography. Gastrointest Endosc. 1993; 39:450–452. PMID: 8514085.
Article14. Minamoto T, Sawaguchi K, Ogino T, Mai M. Anisakiasis of the colon: report of two cases with emphasis on the diagnostic and therapeutic value of colonoscopy. Endoscopy. 1991; 23:50–52. PMID: 2009841.
Article15. Wittner M, Turner JW, Jacquette G, Ash LR, Salgo MP, Tanowitz HB. Eustrongylidiasis: a parasitic infection acquired by eating sushi. N Engl J Med. 1989; 320:1124–1126. PMID: 2710174.16. Pacios E, Arias-Diaz J, Zuloaga J, Gonzalez-Armengol J, Villarroel P, Balibrea JL. Albendazole for the treatment of anisakiasis ileus. Clin Infect Dis. 2005; 41:1825–1826. PMID: 16288416.
Article17. Moore DA, Girdwood RW, Chiodini PL. Treatment of anisakiasis with albendazole. Lancet. 2002; 360:54. PMID: 12114042.
Article18. Bier JW, Deardoff TL, Jackson GJ, Raybourne RB. Human anisakiasis. Baillieres Clin Trop Med Commun Dis. 1987; 2:723–733.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Anisakiasis Concurrently Invading the Stomach, Ileocecal Valve and Transverse Colon
- A Case of Anisakiasis Concurrently Invading Esophagus and Stomach, and Another Case of Esophageal Anisakiasis
- Anisakiasis of the Colon: Report of Two Cases
- A Case of Gastric Anisakiasis Causing Severe Gastric Ulcer Bleeding
- A Case of Rectal Anisakiasis