Brain Tumor Res Treat.
2013 Oct;1(2):91-94. 10.14791/btrt.2013.1.2.91.
Primary Intracranial Fibrosarcoma Presenting with Hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Konkuk University Medical Center, Seoul, Korea. kohyc@kuh.ac.kr
- 2Department of Radiology, Konkuk University Medical Center, Seoul, Korea.
- 3Department of Pathology, Konkuk University Medical Center, Seoul, Korea.
- KMID: 2048481
- DOI: http://doi.org/10.14791/btrt.2013.1.2.91
Abstract
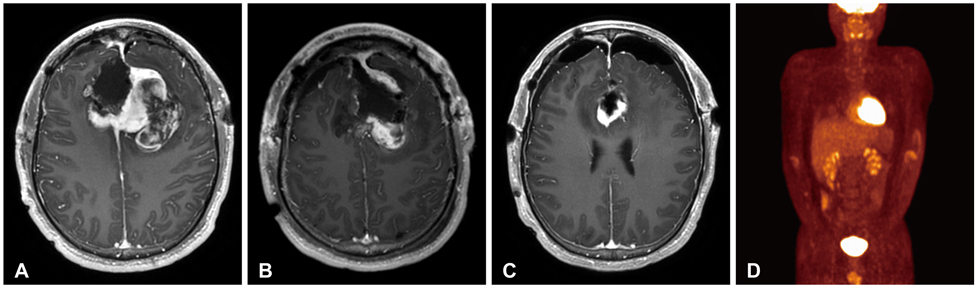
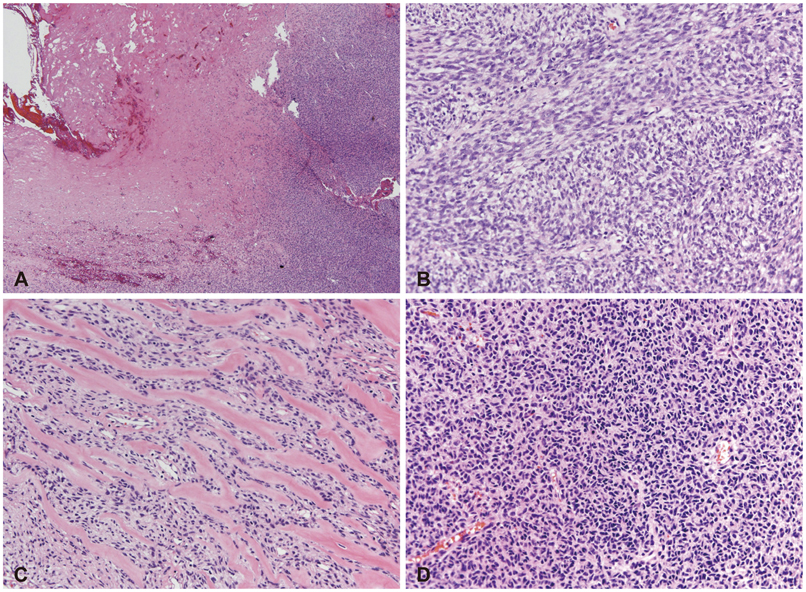
- Primary intracranial fibrosarcomas (PIFs) are extremely rare and the origin of these tumors is still controversial. The rarity of primary intracranial fibrosarcomas makes it difficult to diagnose them correctly and establish a standard treatment. The pathologic diagnosis is made by distinguishing findings from light microscopic and immunohistochemistry analysis. PIFs have been known to be very aggressive neoplasms. The extra-axial location of the tumor could provide an opportunity to perform a total resection even if it does not mean a cure. We present a case of PIFs mimicking a falx meningioma in a 17-year-old man.
MeSH Terms
Figure
Reference
-
1. Chopra R, Bhardwaj M, Premsagar IC. Fibrosarcoma of the meninges. Rare Tumors. 2010; 2:e3.
Article2. Torres G, Petit F, Vilchez V, et al. Primary cerebral fibrosarcoma in a child. Clin Neuropathol. 2007; 26:284–287.
Article3. Bisogno G, Roganovic J, Carli M, et al. Primary intracranial fibrosarcoma. Childs Nerv Syst. 2002; 18:648–651.
Article4. McDonald P, Guha A, Provias J. Primary intracranial fibrosarcoma with intratumoral hemorrhage: neuropathological diagnosis with review of the literature. J Neurooncol. 1997; 35:133–139.5. Vatsal DK, Sharma S, Renjen PN, Kaul S, Jha AN. Primary fibrosarcoma of brain. Neurol India. 2000; 48:396–398.6. Paulus W, Slowik F, Jellinger K. Primary intracranial sarcomas: histopathological features of 19 cases. Histopathology. 1991; 18:395–402.
Article7. Donnet A, Figarella-Branger D, Grisoli F. Primary meningeal fibrosarcoma: a particular neuroradiological presentation. J Neurooncol. 1999; 42:79–83.8. Cai N, Kahn LB. A report of primary brain fibrosarcoma with literature review. J Neurooncol. 2004; 68:161–167.
Article