Brain Tumor Res Treat.
2013 Oct;1(2):64-70. 10.14791/btrt.2013.1.2.64.
Outcome of Surgical Resection of Symptomatic Cerebral Lesions in Non-Small Cell Lung Cancer Patients with Multiple Brain Metastases
- Affiliations
-
- 1NeuroOncology Clinic, Research Institute and Hospital, National Cancer Center, Goyang, Korea. heonyoo@ncc.re.kr
- KMID: 2048477
- DOI: http://doi.org/10.14791/btrt.2013.1.2.64
Abstract
OBJECTIVE
Patients with symptomatic brain metastases secondary to mass effect are often candidates for surgery. However, many of these surgical candidates are also found to have multiple asymptomatic tumors. This study aimed to determine the outcome of surgical resection of symptomatic brain metastases followed by chemotherapy or radiotherapy (RT) for the remnant asymptomatic lesions in non-small cell lung cancer (NSCLC) patients with multiple brain metastases.
METHODS
We conducted a retrospective review of the medical records of 51 NSCLC patients with symptomatic multiple brain metastases who underwent surgical resection, of whom 38 had one or more unresected asymptomatic lesions subsequently treated with chemotherapy and/or RT. Thirteen patients underwent resection of all metastatic lesions.
RESULTS
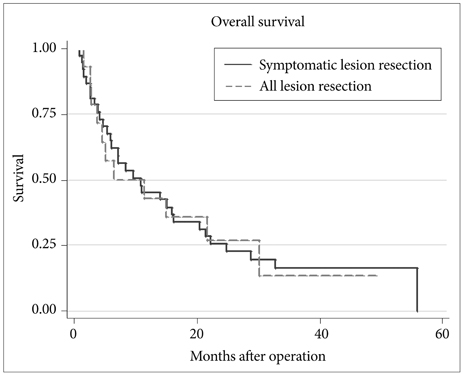
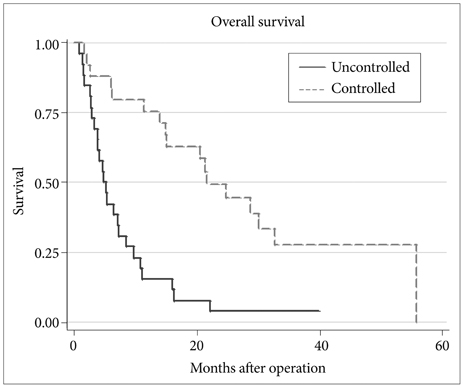
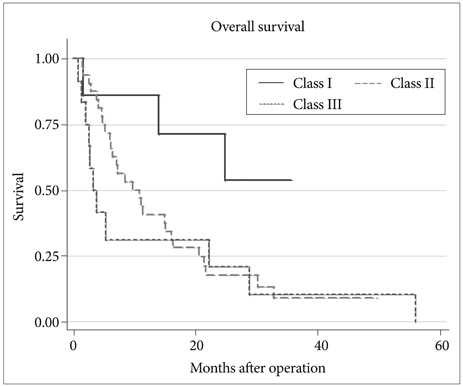
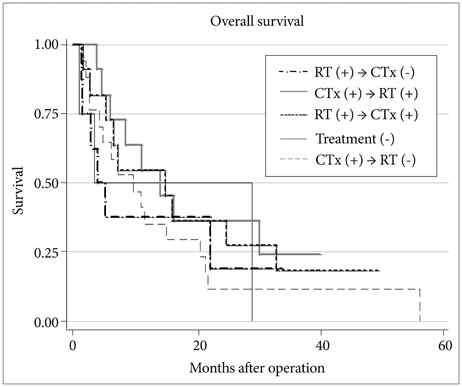
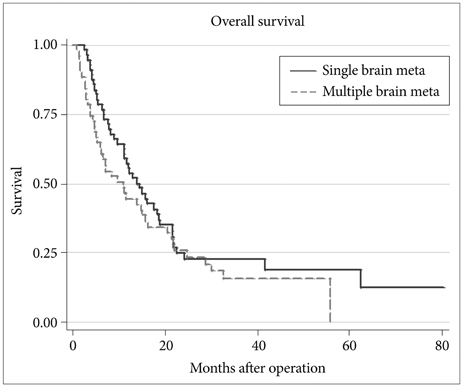
Median survival for overall patient population after surgical resection was 10.8 months. Median survival for patients with surgical resection of all brain metastases was not significantly different with patients who underwent surgical resection of only symptomatic lesions (6.5 months vs. 10.8 months; p=0.97). There was no statistically significant difference in survival according to the number of tumors (p=0.86, 0.16), or post-surgical treatment modalities (p=0.69).
CONCLUSION
The survival time of NSCLC patients with multiple brain metastases after surgery for only symptomatic brain metastases is similar to that of patients who underwent surgery for all brain metastases. The remaining asymptomatic lesions may be treated with chemotherapy or radiotherapy. The optimal treatment modality, however, needs to be defined in prospective trials with larger patient cohort.
Keyword
MeSH Terms
Figure
Reference
-
1. Tsukada Y, Fouad A, Pickren JW, Lane WW. Central nervous system metastasis from breast carcinoma. Autopsy study. Cancer. 1983; 52:2349–2354.
Article2. Arbit E, Wronski M. Clinical decision making in brain metastases. Neurosurg Clin N Am. 1996; 7:447–457.
Article3. Delattre JY, Krol G, Thaler HT, Posner JB. Distribution of brain metastases. Arch Neurol. 1988; 45:741–744.
Article4. Posner JB, Chernik NL. Intracranial metastases from systemic cancer. Adv Neurol. 1978; 19:579–592.5. Amer MH, Al-Sarraf M, Baker LH, Vaitkevicius VK. Malignant melanoma and central nervous system metastases: incidence, diagnosis, treatment and survival. Cancer. 1978; 42:660–668.
Article6. Chason JL, Walker FB, Landers JW. Metastatic carcinoma in the central nervous system and dorsal root ganglia. A prospective autopsy study. Cancer. 1963; 16:781–787.
Article7. Galluzzi S, Payne PM. Brain metastases from primary bronchial carcinoma: a statistical study of 741 necropsies. Br J Cancer. 1956; 10:408–414.
Article8. Rubin P, Brasacchio R, Katz A. Solitary metastases: illusion versus reality. Semin Radiat Oncol. 2006; 16:120–130.
Article9. Seute T, Leffers P, ten Velde GP, Twijnstra A. Detection of brain metastases from small cell lung cancer: consequences of changing imaging techniques (CT versus MRI). Cancer. 2008; 112:1827–1834.
Article10. Cairncross JG, Posner JB. The management of brain metastases. In : Walker MD, editor. Oncology of the Nervous System. Boston: Martinus Nijhoff Publishers;1983. p. 341–377.11. Pollock BE. Management of patients with multiple brain metastases. Contemp Neurosurg. 1999; 21:1–6.
Article12. Kalkanis SN, Kondziolka D, Gaspar LE, et al. The role of surgical resection in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010; 96:33–43.
Article13. Paek SH, Audu PB, Sperling MR, Cho J, Andrews DW. Reevaluation of surgery for the treatment of brain metastases: review of 208 patients with single or multiple brain metastases treated at one institution with modern neurosurgical techniques. Neurosurgery. 2005; 56:1021–1034. discussion 1021-34.14. Stark AM, Tscheslog H, Buhl R, Held-Feindt J, Mehdorn HM. Surgical treatment for brain metastases: prognostic factors and survival in 177 patients. Neurosurg Rev. 2005; 28:115–119.
Article15. Yoo H, Kim YZ, Nam BH, et al. Reduced local recurrence of a single brain metastasis through microscopic total resection. J Neurosurg. 2009; 110:730–736.
Article16. Bindal RK, Sawaya R, Leavens ME, Lee JJ. Surgical treatment of multiple brain metastases. J Neurosurg. 1993; 79:210–216.
Article17. Joseph J, Adler JR, Cox RS, Hancock SL. Linear accelerator-based stereotaxic radiosurgery for brain metastases: the influence of number of lesions on survival. J Clin Oncol. 1996; 14:1085–1092.
Article18. Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys. 1999; 45:427–434.
Article19. Loeffler JS, Alexander E III. Radiosurgery for the treatment of intracranial metastasis. In : Alexander E, Loeffler JS, Lunsford LD, editors. Stereotactic Radiosurgery. New York: Mc-Graw-Hill;1993. p. 197–206.20. Shu HK, Sneed PK, Shiau CY, et al. Factors influencing survival after gamma knife radiosurgery for patients with single and multiple brain metastases. Cancer J Sci Am. 1996; 2:335–342.21. Hazuka MB, Burleson WD, Stroud DN, Leonard CE, Lillehei KO, Kinzie JJ. Multiple brain metastases are associated with poor survival in patients treated with surgery and radiotherapy. J Clin Oncol. 1993; 11:369–373.
Article22. Bonnette P, Puyo P, Gabriel C, et al. Surgical management of non-small cell lung cancer with synchronous brain metastases. Chest. 2001; 119:1469–1475.
Article23. Iwasaki A, Shirakusa T, Yoshinaga Y, Enatsu S, Yamamoto M. Evaluation of the treatment of non-small cell lung cancer with brain metastasis and the role of risk score as a survival predictor. Eur J Cardiothorac Surg. 2004; 26:488–493.
Article24. Abrahams JM, Torchia M, Putt M, Kaiser LR, Judy KD. Risk factors affecting survival after brain metastases from non-small cell lung carcinoma: a follow-up study of 70 patients. J Neurosurg. 2001; 95:595–600.
Article25. Lee DH, Han JY, Kim HT, et al. Primary chemotherapy for newly diagnosed nonsmall cell lung cancer patients with synchronous brain metastases compared with whole-brain radiotherapy administered first: result of a randomized pilot study. Cancer. 2008; 113:143–149.
Article26. Kim KH, Lee J, Lee JI, et al. Can upfront systemic chemotherapy replace stereotactic radiosurgery or whole brain radiotherapy in the treatment of non-small cell lung cancer patients with asymptomatic brain metastases? Lung Cancer. 2010; 68:258–263.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis on the Brain Metastases of Bronchogenic Carcinoma
- Radiotherapy of Brain Metastases from Lung Cancer
- Comparison of Stereotactic Radiosurgery and Whole Brain Radiotherapy in Patients with Four or More Brain Metastases
- Durable response to first-line treatment with AZD3759 (zorifertinib) in a patient with epithelial growth factor receptor mutated non-small cell lung cancer and untreated multiple brain metastasis
- Resection for Pancreatic Cancer Lung Metastases