Use of cryopreserved cadaveric arterial allograft as a vascular conduit for peripheral arterial graft infection
- Affiliations
-
- 1Gachon University of Medicine and Science, Incheon, Korea.
- 2Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ypcho@amc.seoul.kr
- 3Department of Plastic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Surgery, Ulsan University Hospital, Ulsan, Korea.
- KMID: 2047715
- DOI: http://doi.org/10.4174/astr.2015.89.1.51
Abstract
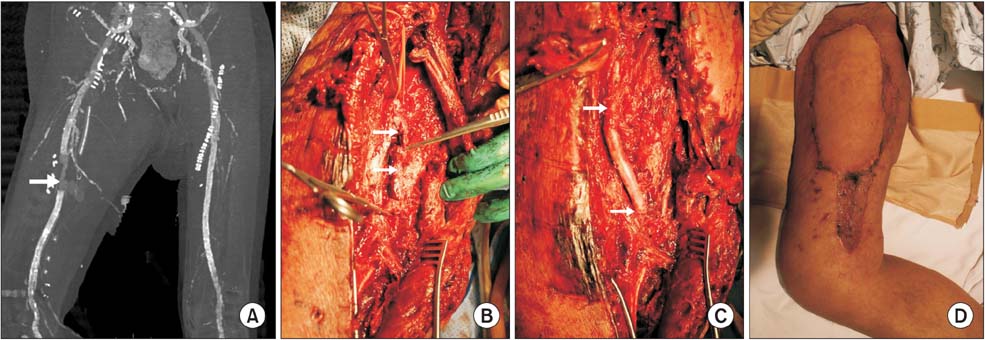
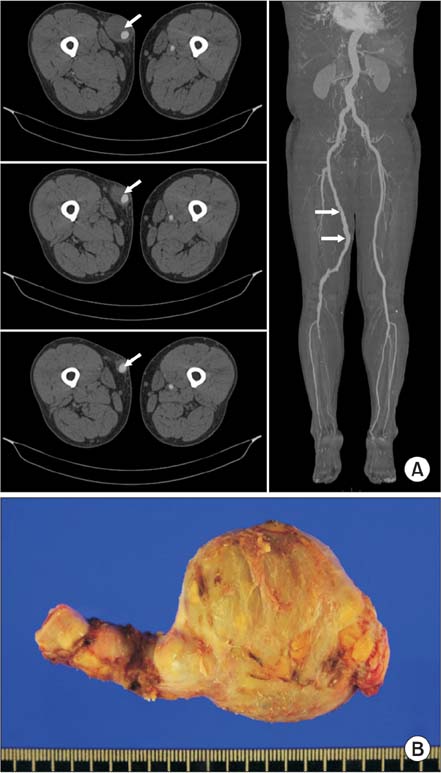
- Major peripheral arterial graft infection is a potentially devastating complication of vascular surgery, associated with significant mortality and high amputation rates. Autologous saphenous veins are considered optimal arterial conduits for lower extremity revascularization in infected fields, but they are often unavailable or unsuitable in these patients. This study describes two patients with major peripheral graft infection, but without available autologous veins, who underwent graft excision and cryopreserved cadaveric arterial allograft reconstruction. Although long-term graft durability is unclear because of gradual deterioration and degeneration, these findings suggest that cadaveric allografts may be good options for patients with major peripheral graft infection.
MeSH Terms
Figure
Cited by 6 articles
-
Graft outflow vein venoplasty for a laparoscopically harvested left lateral section graft in pediatric living donor liver transplantation
Jung-Man Namgoong, Shin Hwang, Ki-Hum Kim, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh, Hyunhee Kwon, Yong Jae Kwon
Korean J Transplant. 2020;34(3):210-216. doi: 10.4285/kjt.2020.34.3.210.Pediatric liver transplantation with hyperreduced left lateral segment graft
Jung-Man Namgoong, Shin Hwang, Gi-Won Song, Dae-Yeon Kim, Tae-Yong Ha, Dong-Hwan Jung, Gil-Chun Park, Chul-Soo Ahn, Kyung Mo Kim, Seak Hee Oh, Hyunhee Kwon, Yong Jae Kwon
Ann Hepatobiliary Pancreat Surg. 2020;24(4):503-512. doi: 10.14701/ahbps.2020.24.4.503.Hilar portal vein wedge resection and patch venoplasty in patients undergoing bile duct resection for hepatobiliary malignancy: A report of two cases
Sung-Min Kim, Shin Hwang
Ann Hepatobiliary Pancreat Surg. 2021;25(1):132-138. doi: 10.14701/ahbps.2021.25.1.132.Unification venoplasty of the outflow hepatic vein for laparoscopically harvested left liver grafts in pediatric living donor liver transplantation
Jung-Man Namgoong, Shin Hwang, Ki-Hun Kim, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh, Hwui-Dong Cho, Hyunhee Kwon, Yong Jae Kwon
Korean J Transplant. 2020;34(4):293-301. doi: 10.4285/kjt.20.0027.Dextroplantation of a reduced left lateral section graft in an infant undergoing living donor liver transplantation
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh, Hyunhee Kwon, Yong Jae Kwon
Ann Hepatobiliary Pancreat Surg. 2021;25(3):414-418. doi: 10.14701/ahbps.2021.25.3.414.Portal vein wedge resection and patch venoplasty using autologous and homologous vein grafts during surgery for hepatobiliary malignancies
Byeong-Gon Na, Shin Hwang, Dong-Hwan Jung, Sung-Gyu Lee
Ann Hepatobiliary Pancreat Surg. 2021;25(4):509-516. doi: 10.14701/ahbps.2021.25.4.509.
Reference
-
1. McCready RA, Bryant MA, Divelbiss J, Wack MF, Mattison HR. Case study: chronic femoropopliteal prosthetic graft infection with exposed graft. Vasc Endovascular Surg. 2009; 43:291–294.2. Reilly LM, Stoney RJ, Goldstone J, Ehrenfeld WK. Improved management of aortic graft infection: the influence of operation sequence and staging. J Vasc Surg. 1987; 5:421–431.3. Castier Y, Paraskevas N, Maury JM, Karsenti A, Cerceau O, Legendre AF, et al. Cryopreserved arterial allograft reconstruction for infected peripheral bypass. Ann Vasc Surg. 2010; 24:994–999.4. Szilagyi DE, Mcdonald RT, Smith RF, Whitcomb JG. Biologic fate of human arterial homografts. AMA Arch Surg. 1957; 75:506–527.5. Meade JW, Linton RR, Darling RC, Menendez CV. Arterial homografts: a long-term clinical follow-up. Arch Surg. 1966; 93:392–399.6. Axthelm SC, Porter JM, Strickland S, Baur GM. Antigenicity of venous allografts. Ann Surg. 1979; 189:290–293.7. Schmitz-Rixen T, Megerman J, Colvin RB, Williams AM, Abbott WM. Immunosuppressive treatment of aortic allografts. J Vasc Surg. 1988; 7:82–92.8. Bia D, Pessana F, Armentano R, Perez H, Graf S, Zocalo Y, et al. Cryopreservation procedure does not modify human carotid homografts mechanical properties: an isobaric and dynamic analysis. Cell Tissue Bank. 2006; 7:183–194.9. Chiesa R, Astore D, Piccolo G, Melissano G, Jannello A, Frigerio D, et al. Fresh and cryopreserved arterial homografts in the treatment of prosthetic graft infections: experience of the Italian Collaborative Vascular Homograft Group. Ann Vasc Surg. 1998; 12:457–462.10. Kieffer E, Gomes D, Chiche L, Fleron MH, Koskas F, Bahnini A. Allograft replacement for infrarenal aortic graft infection: early and late results in 179 patients. J Vasc Surg. 2004; 39:1009–1017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcomes of Cryopreserved Arterial Allograft Used as a Vascular Conduit for Hemodialysis
- Deep Vein as a Graft Conduit
- Comparison of Patency and Viability in Fresh and Cryopreserved Arterialand Venous Allograft Conduits in Dogs
- Flow Cytometric Analysis of Endothelial Cell Viability in Arterial Allograft
- An Experimental Evaluation of Microvascular Grafts