Anat Cell Biol.
2013 Dec;46(4):291-295. 10.5115/acb.2013.46.4.291.
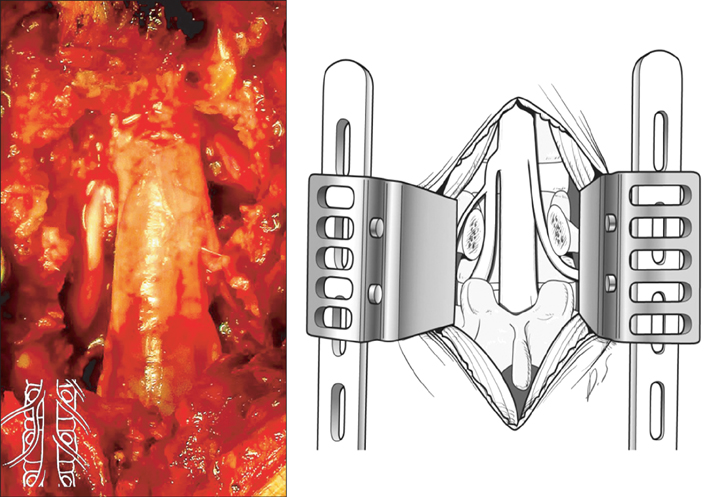
Radiological anatomical consideration of conjoined nerve root with a case review
- Affiliations
-
- 1Department of Neurosurgery, Guro Teun Teun Hospital, Seoul, Korea.
- 2Department of Neurosurgery, Daegu Teun Teun Hospital, Daegu, Korea.
- 3Department of Radiology, Guro Teun Teun Hospital, Seoul, Korea.
- 4Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea. jivago91@hanmail.net
- KMID: 2046770
- DOI: http://doi.org/10.5115/acb.2013.46.4.291
Abstract
- Nerve root anomalies are frequently underrecognized regardless of the advances in imaging studies; they are also underappreciated and underreported when encountered surgically. The classification of conjoined nerve roots is based on whether the nerve root emerges at an abnormal level or from an anastomotic branch. In the present report, we describe case with a conjoined nerve root that emerged at a more caudal level than that normally observed that was an undiagnosed on preoperative imaging studies. We also discuss the atypical imaging features obtained through preoperative imaging studies. As observed in the present case, preoperative recognition and diagnosis of such anomalies offer the best opportunity of performing a successful procedure and preventing inadvertent damage to nerve roots intraoperatively.
Keyword
MeSH Terms
Figure
Reference
-
1. Trimba R, Spivak JM, Bendo JA. Conjoined nerve roots of the lumbar spine. Spine J. 2012; 12:515–524.2. Scuderi GJ, Vaccaro AR, Brusovanik GV, Kwon BK, Berta SC. Conjoined lumbar nerve roots: a frequently underappreciated congenital abnormality. J Spinal Disord Tech. 2004; 17:86–93.3. Postacchini F, Urso S, Ferro L. Lumbosacral nerve-root anomalies. J Bone Joint Surg Am. 1982; 64:721–729.4. Lotan R, Al-Rashdi A, Yee A, Finkelstein J. Clinical features of conjoined lumbosacral nerve roots versus lumbar intervertebral disc herniations. Eur Spine J. 2010; 19:1094–1098.5. White JG 3rd, Strait TA, Binkley JR, Hunter SE. Surgical treatment of 63 cases of conjoined nerve roots. J Neurosurg. 1982; 56:114–117.6. Phillips LH 2nd, Park TS. The frequency of intradural conjoined lumbosacral dorsal nerve roots found during selective dorsal rhizotomy. Neurosurgery. 1993; 33:88–90.7. Artico M, Carloia S, Piacentini M, Ferretti G, Dazzi M, Franchitto S, Bronzetti E. Conjoined lumbosacral nerve roots: observations on three cases and review of the literature. Neurocirugia (Astur). 2006; 17:54–59.8. Gomez JG, Dickey JW, Bachow TB. Conjoined lumbosacral nerve roots. Acta Neurochir (Wien). 1993; 120:155–158.9. Kang CH, Shin MJ, Kim SM, Lee SH, Kim HK, Ryu JA, Lee CS, Kim SS. Conjoined lumbosacral nerve roots compromised by disk herniation: sagittal shoulder sign for the preoperative diagnosis. Skeletal Radiol. 2008; 37:225–231.10. Song SJ, Lee JW, Choi JY, Hong SH, Kim NR, Kim KJ, Chung SK, Kim HJ, Kang HS. Imaging features suggestive of a conjoined nerve root on routine axial MRI. Skeletal Radiol. 2008; 37:133–138.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conjoined Nerve Root Anomaly Associated with Lumbar Disc Herniation: A Case Report
- Conjoined Lumbosacral Nerve Roots without Disc Herniation: Case Report
- Two Cases of Conjoined Twins
- A Case of the Redundant Nerve Root Syndrome Mimicking Intradural Spinal Tumor
- Conjoint Nerve Root an Intraoperative Challenge in Minimally Invasive Tubular Discectomy