Anat Cell Biol.
2012 Sep;45(3):141-148. 10.5115/acb.2012.45.3.141.
Mechanism of experimental autoimmune encephalomyelitis in Lewis rats: recent insights from macrophages
- Affiliations
-
- 1Department of Veterinary Anatomy, Veterinary Medical Research Institute, College of Veterinary Medicine, Jeju National University, Jeju, Korea. shint@jejunu.ac.kr
- 2Functional and Systems Neurobiology, Cajal Institute, Madrid, Spain.
- 3Department of Anatomy, School of Medicine, Jeju National University, Jeju, Korea.
- 4Department of Immunotherapy Development, Tokyo Metropolitan Institute of Medical Science, Tokyo, Japan.
- KMID: 2046740
- DOI: http://doi.org/10.5115/acb.2012.45.3.141
Abstract
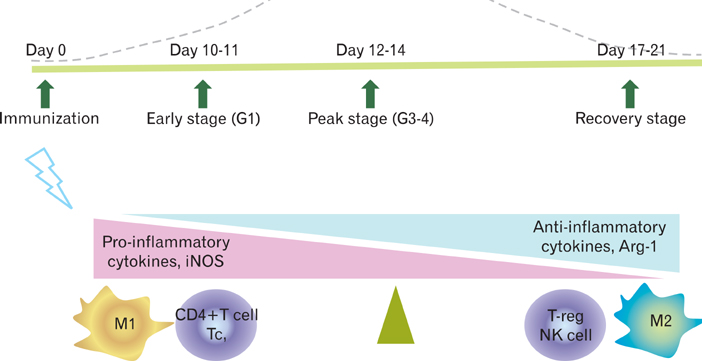
- Experimental autoimmune encephalomyelitis (EAE) in Lewis rats is an acute monophasic paralytic central nervous system disease, in which most rats spontaneously recover from paralysis. EAE in Lewis rats is induced by encephalitogenic antigens, including myelin basic protein. EAE is mediated by CD4+ Th1 cells, which secrete pro-inflammatory mediators, and spontaneous recovery is mediated by regulatory T cells. Recently, it was established that classically activated macrophages (M1 phenotype) play an important role in the initiation of EAE, while alternatively activated macrophages (M2 phenotype) contribute to spontaneous recovery from rat EAE. This review will summarize the neuroimmunological aspects of active monophasic EAE, which manifests as neuroinflammation followed by neuroimmunomodulation and/or neuroprotection, with a focus on the role of alternatively activated macrophages.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Amelioration of experimental autoimmune encephalomyelitis by Ishige okamurae
Meejung Ahn, Jeongtae Kim, Wonjun Yang, Yuna Choi, Poornima Ekanayake, Hyunju Ko, Youngheun Jee, Taekyun Shin
Anat Cell Biol. 2018;51(4):292-298. doi: 10.5115/acb.2018.51.4.292.
Reference
-
1. Stadelmann C, Wegner C, Brück W. Inflammation, demyelination, and degeneration: recent insights from MS pathology. Biochim Biophys Acta. 2011. 1812:275–282.2. Herz J, Zipp F, Siffrin V. Neurodegeneration in autoimmune CNS inflammation. Exp Neurol. 2010. 225:9–17.3. Kapadia M, Sakic B. Autoimmune and inflammatory mechanisms of CNS damage. Prog Neurobiol. 2011. 95:301–333.4. Wekerle H. Lessons from multiple sclerosis: models, concepts, observations. Ann Rheum Dis. 2008. 67:Suppl 3. iii56–iii60.5. Mix E, Meyer-Rienecker H, Hartung HP, Zettl UK. Animal models of multiple sclerosis: potentials and limitations. Prog Neurobiol. 2010. 92:386–404.6. Willenborg DO, Staykova MA, Cowden WB. Our shifting understanding of the role of nitric oxide in autoimmune encephalomyelitis: a review. J Neuroimmunol. 1999. 100:21–35.7. Batoulis H, Addicks K, Kuerten S. Emerging concepts in autoimmune encephalomyelitis beyond the CD4/T(H)1 paradigm. Ann Anat. 2010. 192:179–193.8. Markovic M, Miljkovic D, Momcilovic M, Popadic D, Miljkovic Z, Savic E, Ramic Z, Mostarica Stojkovic M. Strain difference in susceptibility to experimental autoimmune encephalomyelitis in rats correlates with T(H)1 and T(H)17-inducing cytokine profiles. Mol Immunol. 2009. 47:141–146.9. Stosic-Grujicic S, Ramic Z, Bumbasirevic V, Harhaji L, Mostarica-Stojkovic M. Induction of experimental autoimmune encephalomyelitis in Dark Agouti rats without adjuvant. Clin Exp Immunol. 2004. 136:49–55.10. Papadopoulos D, Pham-Dinh D, Reynolds R. Axon loss is responsible for chronic neurological deficit following inflammatory demyelination in the rat. Exp Neurol. 2006. 197:373–385.11. Ahn M, Yang W, Kim H, Jin JK, Moon C, Shin T. Immunohistochemical study of arginase-1 in the spinal cords of Lewis rats with experimental autoimmune encephalomyelitis. Brain Res. 2012. 1453:77–86.12. Shin T, Kojima T, Tanuma N, Ishihara Y, Matsumoto Y. The subarachnoid space as a site for precursor T cell proliferation and effector T cell selection in experimental autoimmune encephalomyelitis. J Neuroimmunol. 1995. 56:171–178.13. Mannie M, Swanborg RH, Stepaniak JA. Experimental autoimmune encephalomyelitis in the rat. Curr Protoc Immunol. 2009. Chapter 15:Unit 15.2.14. Ohmori K, Hong Y, Fujiwara M, Matsumoto Y. In situ demonstration of proliferating cells in the rat central nervous system during experimental autoimmune encephalomyelitis: evidence suggesting that most infiltrating T cells do not proliferate in the target organ. Lab Invest. 1992. 66:54–62.15. Matsumoto Y, Fujiwara M. The immunopathology of adoptively transferred experimental allergic encephalomyelitis (EAE) in Lewis rats. Part 1. Immunohistochemical examination of developing lesions of EAE. J Neurol Sci. 1987. 77:35–47.16. Dimitriadou V, Pang X, Theoharides TC. Hydroxyzine inhibits experimental allergic encephalomyelitis (EAE) and associated brain mast cell activation. Int J Immunopharmacol. 2000. 22:673–684.17. Swanborg RH, Stepaniak JA. Experimental autoimmune encephalomyelitis in the rat. Curr Protoc Immunol. 2001. Chapter 15:Unit 15.2.18. Swanborg RH. Experimental autoimmune encephalomyelitis in the rat: lessons in T-cell immunology and autoreactivity. Immunol Rev. 2001. 184:129–135.19. Tanuma N, Shin T, Matsumoto Y. Characterization of acute versus chronic relapsing autoimmune encephalomyelitis in DA rats. J Neuroimmunol. 2000. 108:171–180.20. Moon C, Ahn M, Wie MB, Kim HM, Koh CS, Hong SC, Kim MD, Tanuma N, Matsumoto Y, Shin T. Phenidone, a dual inhibitor of cyclooxygenases and lipoxygenases, ameliorates rat paralysis in experimental autoimmune encephalomyelitis by suppressing its target enzymes. Brain Res. 2005. 1035:206–210.21. Moon C, Ahn M, Jee Y, Heo S, Kim S, Kim H, Sim KB, Koh CS, Shin YG, Shin T. Sodium salicylate-induced amelioration of experimental autoimmune encephalomyelitis in Lewis rats is associated with the suppression of inducible nitric oxide synthase and cyclooxygenases. Neurosci Lett. 2004. 356:123–126.22. Ahn M, Kang J, Lee Y, Riu K, Kim Y, Jee Y, Matsumoto Y, Shin T. Pertussis toxin-induced hyperacute autoimmune encephalomyelitis in Lewis rats is correlated with increased expression of inducible nitric oxide synthase and tumor necrosis factor alpha. Neurosci Lett. 2001. 308:41–44.23. Schneider C, Schuetz G, Zollner TM. Acute neuroinflammation in Lewis rats: a model for acute multiple sclerosis relapses. J Neuroimmunol. 2009. 213:84–90.24. Mandolesi G, Grasselli G, Musumeci G, Centonze D. Cognitive deficits in experimental autoimmune encephalomyelitis: neuroinflammation and synaptic degeneration. Neurol Sci. 2010. 31:Suppl 2. S255–S259.25. Berrendero F, Sánchez A, Cabranes A, Puerta C, Ramos JA, García-Merino A, Fernández-Ruiz J. Changes in cannabinoid CB(1) receptors in striatal and cortical regions of rats with experimental allergic encephalomyelitis, an animal model of multiple sclerosis. Synapse. 2001. 41:195–202.26. Pender MP, Tabi Z, Nguyen KB, McCombe PA. The proximal peripheral nervous system is a major site of demyelination in experimental autoimmune encephalomyelitis induced in the Lewis rat by a myelin basic protein-specific T cell clone. Acta Neuropathol. 1995. 89:527–531.27. Tsuchida M, Matsumoto Y, Hirahara H, Hanawa H, Tomiyama K, Abo T. Preferential distribution of V beta 8.2-positive T cells in the central nervous system of rats with myelin basic protein-induced autoimmune encephalomyelitis. Eur J Immunol. 1993. 23:2399–2406.28. Polfliet MM, van de Veerdonk F, Döpp EA, van Kesteren-Hendrikx EM, van Rooijen N, Dijkstra CD, van den Berg TK. The role of perivascular and meningeal macrophages in experimental allergic encephalomyelitis. J Neuroimmunol. 2002. 122:1–8.29. Benveniste EN. Role of macrophages/microglia in multiple sclerosis and experimental allergic encephalomyelitis. J Mol Med (Berl). 1997. 75:165–173.30. Matsumoto Y, Tsuchida M, Hanawa H, Abo T. Successful prevention and treatment of autoimmune encephalomyelitis by short-term administration of anti-T-cell receptor alpha beta antibody. Immunology. 1994. 81:1–7.31. Imrich H, Kugler C, Torres-Nagel N, Dörries R, Hünig T. Prevention and treatment of Lewis rat experimental allergic encephalomyelitis with a monoclonal antibody to the T cell receptor V beta 8.2 segment. Eur J Immunol. 1995. 25:1960–1964.32. Jung S, Huitinga I, Schmidt B, Zielasek J, Dijkstra CD, Toyka KV, Hartung HP. Selective elimination of macrophages by dichlormethylene diphosphonate-containing liposomes suppresses experimental autoimmune neuritis. J Neurol Sci. 1993. 119:195–202.33. Huitinga I, Damoiseaux JG, Döpp EA, Dijkstra CD. Treatment with anti-CR3 antibodies ED7 and ED8 suppresses experimental allergic encephalomyelitis in Lewis rats. Eur J Immunol. 1993. 23:709–715.34. Tanuma N, Kojima T, Shin T, Aikawa Y, Kohji T, Ishihara Y, Matsumoto Y. Competitive PCR quantification of pro- and anti-inflammatory cytokine mRNA in the central nervous system during autoimmune encephalomyelitis. J Neuroimmunol. 1997. 73:197–206.35. Tanuma N, Shin T, Kogure K, Matsumoto Y. Differential role of TNF-alpha and IFN-gamma in the brain of rats with chronic relapsing autoimmune encephalomyelitis. J Neuroimmunol. 1999. 96:73–79.36. Goverman J. Autoimmune T cell responses in the central nervous system. Nat Rev Immunol. 2009. 9:393–407.37. Körner H, Lemckert FA, Chaudhri G, Etteldorf S, Sedgwick JD. Tumor necrosis factor blockade in actively induced experimental autoimmune encephalomyelitis prevents clinical disease despite activated T cell infiltration to the central nervous system. Eur J Immunol. 1997. 27:1973–1981.38. Huitinga I, Schmidt ED, van der Cammen MJ, Binnekade R, Tilders FJ. Priming with interleukin-1beta suppresses experimental allergic encephalomyelitis in the Lewis rat. J Neuroendocrinol. 2000. 12:1186–1193.39. Bauer J, Berkenbosch F, Van Dam AM, Dijkstra CD. Demonstration of interleukin-1 beta in Lewis rat brain during experimental allergic encephalomyelitis by immunocytochemistry at the light and ultrastructural level. J Neuroimmunol. 1993. 48:13–21.40. Linker RA, Lühder F, Kallen KJ, Lee DH, Engelhardt B, Rose-John S, Gold R. IL-6 transsignalling modulates the early effector phase of EAE and targets the blood-brain barrier. J Neuroimmunol. 2008. 205:64–72.41. Kiefer R, Schweitzer T, Jung S, Toyka KV, Hartung HP. Sequential expression of transforming growth factor-beta1 by T-cells, macrophages, and microglia in rat spinal cord during autoimmune inflammation. J Neuropathol Exp Neurol. 1998. 57:385–395.42. Rott O, Fleischer B, Cash E. Interleukin-10 prevents experimental allergic encephalomyelitis in rats. Eur J Immunol. 1994. 24:1434–1440.43. Kruglov AA, Lampropoulou V, Fillatreau S, Nedospasov SA. Pathogenic and protective functions of TNF in neuroinflammation are defined by its expression in T lymphocytes and myeloid cells. J Immunol. 2011. 187:5660–5670.44. Matsumoto Y, Sakuma H, Kohyama K, Park IK. Paralysis of CD4(+)CD25(+) regulatory T cell response in chronic autoimmune encephalomyelitis. J Neuroimmunol. 2007. 187:44–54.45. Matsumoto Y, Kohyama K, Aikawa Y, Shin T, Kawazoe Y, Suzuki Y, Tanuma N. Role of natural killer cells and TCR gamma delta T cells in acute autoimmune encephalomyelitis. Eur J Immunol. 1998. 28:1681–1688.46. Kim S, Moon C, Wie MB, Kim H, Tanuma N, Matsumoto Y, Shin T. Enhanced expression of constitutive and inducible forms of nitric oxide synthase in autoimmune encephalomyelitis. J Vet Sci. 2000. 1:11–17.47. Moon C, Kim S, Wie M, Kim H, Cheong J, Park J, Jee Y, Tanuma N, Matsumoto Y, Shin T. Increased expression of p53 and Bax in the spinal cords of rats with experimental autoimmune encephalomyelitis. Neurosci Lett. 2000. 289:41–44.48. Almolda B, González B, Castellano B. Activated microglial cells acquire an immature dendritic cell phenotype and may terminate the immune response in an acute model of EAE. J Neuroimmunol. 2010. 223:39–54.49. Almolda B, Gonzalez B, Castellano B. Antigen presentation in EAE: role of microglia, macrophages and dendritic cells. Front Biosci. 2011. 16:1157–1171.50. Almolda B, Costa M, Montoya M, González B, Castellano B. Increase in Th17 and T-reg lymphocytes and decrease of IL22 correlate with the recovery phase of acute EAE in rat. PLoS One. 2011. 6:e27473.51. Tischner D, Weishaupt A, van den Brandt J, Müller N, Beyersdorf N, Ip CW, Toyka KV, Hünig T, Gold R, Kerkau T, Reichardt HM. Polyclonal expansion of regulatory T cells interferes with effector cell migration in a model of multiple sclerosis. Brain. 2006. 129:2635–2647.52. Bettini M, Vignali DA. Regulatory T cells and inhibitory cytokines in autoimmunity. Curr Opin Immunol. 2009. 21:612–618.53. Shin T, Matsumoto Y. A quantitative analysis of CD45Rlow CD4+ T cells in the subarachnoid space of Lewis rats with autoimmune encephalomyelitis. Immunol Invest. 2001. 30:57–64.54. Matsumoto Y, Abe S, Tsuchida M, Hirahara H, Abo T, Shin T, Tanuma N, Kojima T, Ishihara Y. Characterization of CD4-CD8-T cell receptor alpha beta + T cells appearing in the subarachnoid space of rats with autoimmune encephalomyelitis. Eur J Immunol. 1996. 26:1328–1334.55. Damoiseaux JG, Döpp EA, Neefjes JJ, Beelen RH, Dijkstra CD. Heterogeneity of macrophages in the rat evidenced by variability in determinants: two new anti-rat macrophage antibodies against a heterodimer of 160 and 95 kd (CD11/CD18). J Leukoc Biol. 1989. 46:556–564.56. Damoiseaux JG, Döpp EA, Beelen RH, Dijkstra CD. Rat bone marrow and monocyte cultures: influence of culture time and lymphokines on the expression of macrophage differentiation antigens. J Leukoc Biol. 1989. 46:246–253.57. Martinez FO, Sica A, Mantovani A, Locati M. Macrophage activation and polarization. Front Biosci. 2008. 13:453–461.58. Matsumoto Y, Ohmori K, Fujiwara M. Microglial and astroglial reactions to inflammatory lesions of experimental autoimmune encephalomyelitis in the rat central nervous system. J Neuroimmunol. 1992. 37:23–33.59. Napoli I, Neumann H. Protective effects of microglia in multiple sclerosis. Exp Neurol. 2010. 225:24–28.60. Almolda B, Costa M, Montoya M, González B, Castellano B. CD4 microglial expression correlates with spontaneous clinical improvement in the acute Lewis rat EAE model. J Neuroimmunol. 2009. 209:65–80.61. Mikita J, Dubourdieu-Cassagno N, Deloire MS, Vekris A, Biran M, Raffard G, Brochet B, Canron MH, Franconi JM, Boiziau C, Petry KG. Altered M1/M2 activation patterns of monocytes in severe relapsing experimental rat model of multiple sclerosis. Amelioration of clinical status by M2 activated monocyte administration. Mult Scler. 2011. 17:2–15.62. Dheen ST, Kaur C, Ling EA. Microglial activation and its implications in the brain diseases. Curr Med Chem. 2007. 14:1189–1197.63. Polazzi E, Monti B. Microglia and neuroprotection: from in vitro studies to therapeutic applications. Prog Neurobiol. 2010. 92:293–315.64. Weber MS, Prod'homme T, Youssef S, Dunn SE, Rundle CD, Lee L, Patarroyo JC, Stüve O, Sobel RA, Steinman L, Zamvil SS. Type II monocytes modulate T cell-mediated central nervous system autoimmune disease. Nat Med. 2007. 13:935–943.65. Kim MD, Cho HJ, Shin T. Expression of osteopontin and its ligand, CD44, in the spinal cords of Lewis rats with experimental autoimmune encephalomyelitis. J Neuroimmunol. 2004. 151:78–84.66. Kang SY, Kang JH, Choi JC, Lee JS, Lee CS, Shin T. Expression of erythropoietin in the spinal cord of lewis rats with experimental autoimmune encephalomyelitis. J Clin Neurol. 2009. 5:39–45.67. Kim H, Moon C, Ahn M, Byun J, Lee Y, Kim MD, Matsumoto Y, Koh CS, Shin T. Heat shock protein 27 upregulation and phosphorylation in rat experimental autoimmune encephalomyelitis. Brain Res. 2009. 1304:155–163.68. Rabie T, Marti HH. Brain protection by erythropoietin: a manifold task. Physiology (Bethesda). 2008. 23:263–274.69. Chen W, Ma Q, Suzuki H, Hartman R, Tang J, Zhang JH. Osteopontin reduced hypoxia-ischemia neonatal brain injury by suppression of apoptosis in a rat pup model. Stroke. 2011. 42:764–769.70. Braitch M, Constantinescu CS. The role of osteopontin in experimental autoimmune encephalomyelitis (EAE) and multiple sclerosis (MS). Inflamm Allergy Drug Targets. 2010. 9:249–256.71. Zhao W, Tilton RG, Corbett JA, McDaniel ML, Misko TP, Williamson JR, Cross AH, Hickey WF. Experimental allergic encephalomyelitis in the rat is inhibited by aminoguanidine, an inhibitor of nitric oxide synthase. J Neuroimmunol. 1996. 64:123–133.72. Cowden WB, Cullen FA, Staykova MA, Willenborg DO. Nitric oxide is a potential down-regulating molecule in autoimmune disease: inhibition of nitric oxide production renders PVG rats highly susceptible to EAE. J Neuroimmunol. 1998. 88:1–8.73. Ponomarev ED, Maresz K, Tan Y, Dittel BN. CNS-derived interleukin-4 is essential for the regulation of autoimmune inflammation and induces a state of alternative activation in microglial cells. J Neurosci. 2007. 27:10714–10721.74. Moon C, Heo S, Ahn M, Kim H, Shin M, Sim KB, Kim HM, Shin T. Immunohistochemical study of osteopontin in the spinal cords of rats with clip compression injury. J Vet Med Sci. 2004. 66:1307–1310.75. Ahn M, Lee C, Jung K, Kim H, Moon C, Sim KB, Shin T. Immunohistochemical study of arginase-1 in the spinal cords of rats with clip compression injury. Brain Res. 2012. 1445:11–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Increased expression of neuronal nitric oxide synthase in astrocytes and macrophages in the spinal cord of Lewis rats with autoimmune encephalomyelitis
- Melatonin ameliorates autoimmune encephalomyelitis through suppression of intercellular adhesion molecule-1
- Expression of Erythropoietin in the Spinal Cord of Lewis Rats with Experimental Autoimmune Encephalomyelitis
- Effects of Dexamethasone on Neurogenic Bladder in Experimental Autoimmune Encephalomyelitis Rat
- Immunohistochemical Localization of Bcl-2 in the Spinal Cords of Rats with Experimental Autoimmune Encephalomyelitis