Chonnam Med J.
2008 Aug;44(2):99-103. 10.4068/cmj.2008.44.2.99.
Surgical Outcomes following Exchange of Opacified Hydrophilic Acrylic Intraocualr Lenses
- Affiliations
-
- 1Department of Ophthalmology, Chonnam National University and Hospital, Gwangju, Korea. kcyoon@chonnam.ac.kr
- 2Best Eye Clinic, Gwangju, Korea.
- 3Chonnam National University Research Institute of Medical Sciences, Gwangju, Korea.
- KMID: 2045757
- DOI: http://doi.org/10.4068/cmj.2008.44.2.99
Abstract
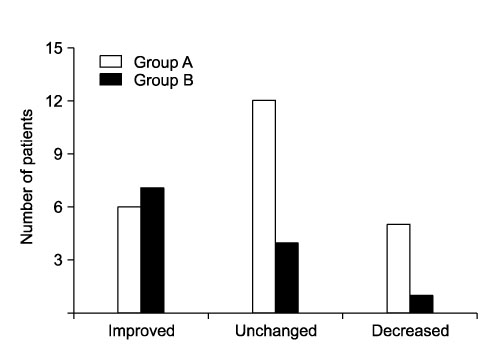
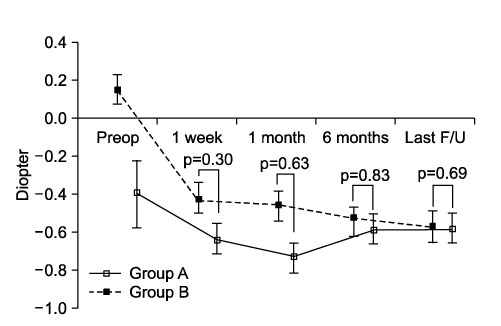
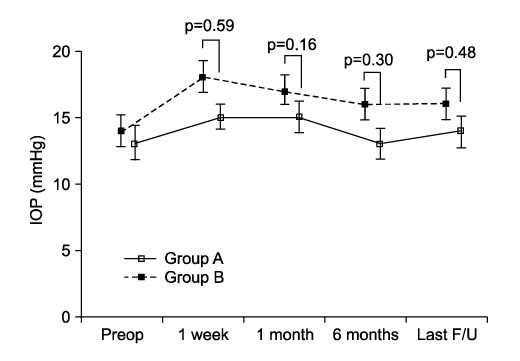
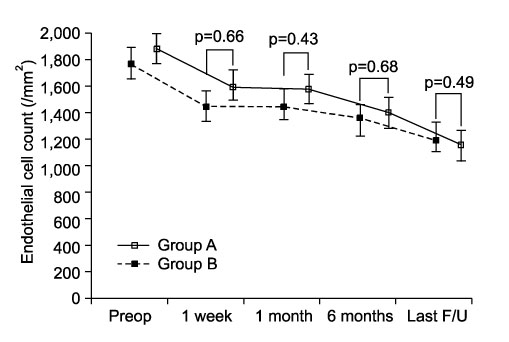
- To evaluate clinical outcomes of opacified Ophthalmed intraocular lens (IOL) exchange according to the intraoperative complications. Thirty-five patients (35 eyes) underwent exchange of Ophthalmed(R) IOLs for late postoperative opacification and were divided into two groups. The IOL exchange procedure was uneventful in 23 eyes (group A), whereas posterior capsular rupture or vitreous loss developed in 12 eyes (group B). The preoperative, and postoperative data were analyzed and compared. The mean interval between the initial surgery and the diagnosis of IOL opacification was 21.05+/-09.26 months (range, 3~43 months). New IOLs were implanted in the capsular bag or sulcus in 25 eyes (71.4%) or by scleral fixation in 10 eyes (28.6%). Following the procedure, the mean logMAR visual acuity (VA) significantly improved from 0.42+/-0.27 to 0.26+/-0.28 (p<0.05). VA improved in 13 eyes (37.1%), remained unchanged in 16 eyes (45.7%). There were no significant differences in changes of refraction, intraocular pressure, and endothelial cell count between group A and B. Although exchange procedure for opacified Ophthalmed IOLs had the risk of intraoperative complications, it could be helpful to improve visual function.
MeSH Terms
Figure
Reference
-
1. Altaie R, Loane E, O'Sullivan k, Beatty S. Surgical and visual outcomes following exchange of opacified Hydroview intraocular lenses. Br J Ophthalmol. 2007. 91:299–302.
Article2. Voros GM, Strong NP. Exchange technique for opacified hydrophilic acrylic intraocular lenses. Eur J Ophthalmol. 2005. 15:465–467.
Article3. Frohn A, Dick HB, Augustin AJ, Grus FH. Late opacification of the foldable hydrophilic acrylic lens SC60B-OUV. Ophthalmology. 2001. 108:1999–2004.
Article4. Gashau AG, Anand A, Chawdhary S. Hydrophilic acrylic intraocular lens exchange: five-year experience. J Cataract Refract Surg. 2006. 32:1340–1344.
Article5. Jin GJ, Crandall AS, Jones JJ. Changing indications for and improving outcomes of intraocular lens exchange. Am J Ophthalmol. 2005. 140:688–694.
Article6. Mamalis N, Davis B, Nilson CD, Hickman MS, Leboyer RM. Complications of foldable intraocular lenses requiring explantation or secondary intervention-2003 survey update. J Cataract Refract Surg. 2004. 30:2209–2218.
Article7. Jirásková N, Rozsival P, Kohout A. A survey of intraocular lens explantation: a retrospective analysis of 23 IOLs explanted during 2005. Eur J Ophthalmol. 2007. 17:579–587.
Article8. Saeed MU, Jafree AJ, de Cock R. Intralenticular opacification of hydrophilic acrylic intraocular lenses. Eye. 2005. 19:661–664.
Article9. Werner L. Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg. 2007. 33:713–726.
Article10. Chang BY, Davey KG, Gupta M, Hutchison C. Late clouding of an acrylic intraocular lens following routine phacoemulsification. Eye. 1999. 13:807–808.
Article11. Kim CY, Kang SJ, Lee SJ, Park SH, Koh HJ. Opacification of a hydrophilic acrylic intraocular lens with exacerbation of Behçet's uveitis. J Cataract Refract Surg. 2002. 28:1276–1278.
Article12. Marques FF, Marques DM, Osher RH, Freitas LL. Longitudinal study of intraocular lens exchange. J Cataract Refract Surg. 2007. 33:254–257.
Article13. Balasubramaniam C, Goodfellow J, Price N, Kirkpatrick N. Opacification of the Hydroview H60M intraocular lens: total patient recall. J Cataract Refract Surg. 2006. 32:944–948.
Article14. Syam P, Byrne P, Lewis G, Husain T, Kleinmann G, Mamalis N, et al. Hydroview lens implant calcification: 186 exchanges at a district general hospital. Eye. 2008. 22:325–331.
Article15. Lee DH, Seo Y, Joo CK. Progressive opacification of hydrophilic acrylic intraocular lenses in diabetic patients. J Cataract Refract Surg. 2002. 28:1271–1275.
Article16. Altaie RW, Costigan T, Donegan S, O'brien P, Mahmood U, Bogdan AJ, et al. Investigation and management of an epidemic of Hydroview intraocular lens opacification. Graefes Arch Clin Exp Ophthalmol. 2005. 243:1124–1133.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Determine a Proper Axial Length by Ultrasonic Biometry in Opaque Hydrophilic Acrylic Intraocular Lens
- Comparision of the Three Different Hydrophilic Acrylic Intraocular Lenses
- The Clinical Outcomes of Lens Exchange in Patients with Opacified Posterior Chamber Lens
- Surgical Results and Complications of Implanted Primary Intraocular Lenses in Pediatric Cataract
- A Clinical Comparison of AcrySof(r) with Hyd rophilic Acrylic IOLs