J Cardiovasc Ultrasound.
2014 Sep;22(3):134-138. 10.4250/jcu.2014.22.3.134.
Infective Endocarditis Associated with Transcatheter Aortic Valve Replacement: Potential Importance of Local Trauma for a Deadly Nidus
- Affiliations
-
- 1Cardiovascular Center and Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. splee0624@gmail.com
- KMID: 2045429
- DOI: http://doi.org/10.4250/jcu.2014.22.3.134
Abstract
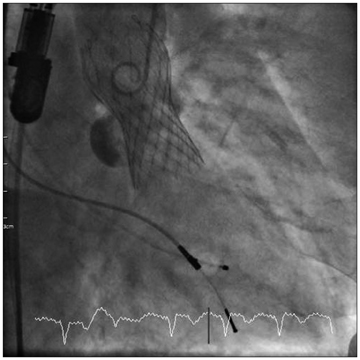
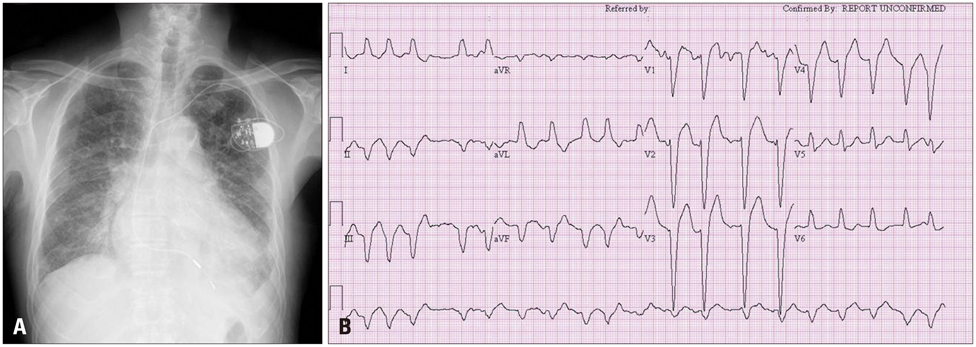
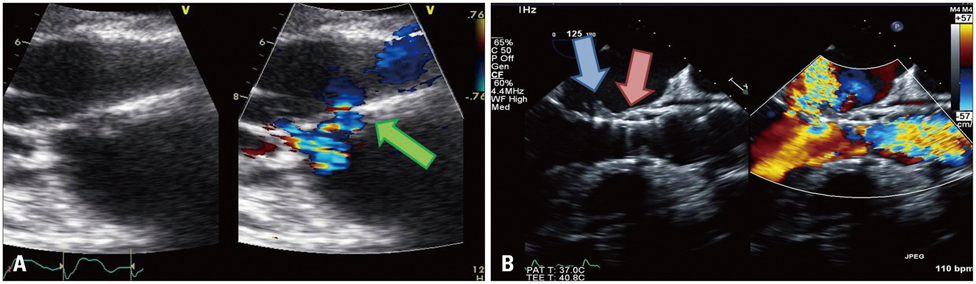
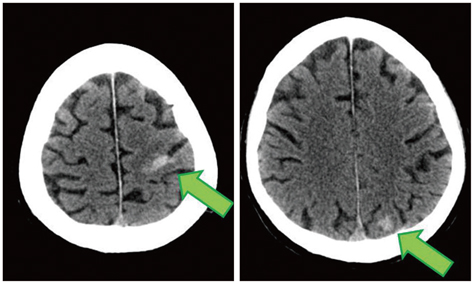
- Recently, transcatheter aortic valve replacement (TAVR) has emerged as an alternative for the treatment of severe symptomatic aortic stenosis patients. Although experience with TAVR is increasing exponentially, few cases of post-TAVR endocarditis are reported. We present a case of 76-year-old man with infective endocarditis after TAVR who was definitely diagnosed by echocardiography.
Figure
Reference
-
1. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ. PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011; 364:2187–2198.
Article2. Loh PH, Bundgaard H, S Ndergaard L. Infective endocarditis following transcatheter aortic valve replacement-: diagnostic and management challenges. Catheter Cardiovasc Interv. 2013; 81:623–627.
Article3. Raschpichler M, Seeburger J, Strasser RH, Misfeld M. Corevalve prosthesis causes anterior mitral leaflet perforation resulting in severe mitral regurgitation and subsequent endocarditis. Eur Heart J. 2014; 35:1587.
Article4. Abdel-Wahab M, Zahn R, Horack M, Gerckens U, Schuler G, Sievert H, Eggebrecht H, Senges J, Richardt G. German transcatheter aortic valve interventions registry investigators. Aortic regurgitation after transcatheter aortic valve implantation: incidence and early outcome. Results from the German transcatheter aortic valve interventions registry. Heart. 2011; 97:899–906.
Article5. Puls M, Eiffert H, Hünlich M, Schöndube F, Hasenfuß G, Seipelt R, Schillinger W. Prosthetic valve endocarditis after transcatheter aortic valve implantation: the incidence in a single-centre cohort and reflections on clinical, echocardiographic and prognostic features. EuroIntervention. 2013; 8:1407–1418.
Article6. Linke A, Wenaweser P, Gerckens U, Tamburino C, Bosmans J, Bleiziffer S, Blackman D, Schäfer U, Müller R, Sievert H, Søndergaard L, Klugmann S, Hoffmann R, Tchétché D, Colombo A, Legrand VM, Bedogni F, Leprince P, Schuler G, Mazzitelli D, Eftychiou C, Frerker C, Boekstegers P, Windecker S, Mohr FW, Woitek F, Lange R, Bauernschmitt R, Brecker S. For the ADVANCE study Investigators. Treatment of aortic stenosis with a self-expanding transcatheter valve: the International Multi-centre ADVANCE Study. Eur Heart J. 2014; [Epub ahead of print].
Article7. Adams DH, Popma JJ, Reardon MJ, Yakubov SJ, Coselli JS, Deeb GM, Gleason TG, Buchbinder M, Hermiller J Jr, Kleiman NS, Chetcuti S, Heiser J, Merhi W, Zorn G, Tadros P, Robinson N, Petrossian G, Hughes GC, Harrison JK, Conte J, Maini B, Mumtaz M, Chenoweth S, Oh JK. U.S. CoreValve Clinical Investigators. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014; 370:1790–1798.
Article8. Carnero-Alcázar M, Maroto Castellanos LC, Carnicer JC, Rodríguez Hernández JE. Transapical aortic valve prosthetic endocarditis. Interact Cardiovasc Thorac Surg. 2010; 11:252–253.
Article9. Eisen A, Shapira Y, Sagie A, Kornowski R. Infective endocarditis in the transcatheter aortic valve replacement era: comprehensive review of a rare complication. Clin Cardiol. 2012; 35:E1–E5.
Article10. Head SJ, Dewey TM, Mack MJ. Fungal endocarditis after transfemoral aortic valve implantation. Catheter Cardiovasc Interv. 2011; 78:1017–1019.
Article11. Wong DR, Boone RH, Thompson CR, Allard MF, Altwegg L, Carere RG, Cheung A, Ye J, Lichtenstein SV, Ling H, Webb JG. Mitral valve injury late after transcatheter aortic valve implantation. J Thorac Cardiovasc Surg. 2009; 137:1547–1549.
Article12. Castiglioni A, Pozzoli A, Maisano F, Alfieri O. Endocarditis after transfemoral aortic valve implantation in a patient with Osler-Weber-Rendu syndrome. Interact Cardiovasc Thorac Surg. 2012; 15:553–554.
Article13. Comoglio C, Boffini M, El Qarra S, Sansone F, D'Amico M, Marra S, Rinaldi M. Aortic valve replacement and mitral valve repair as treatment of complications after percutaneous core valve implantation. J Thorac Cardiovasc Surg. 2009; 138:1025–1027.
Article14. Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, de Jesus Antunes M, Thilen U, Lekakis J, Lengyel M, Müller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL. ESC Committee for Practice Guidelines. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J. 2009; 30:2369–2413.15. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT. American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee. American Heart Association Council on Cardiovascular Disease in the Young. American Heart Association Council on Clinical Cardiology. American Heart Association Council on Cardiovascular Surgery and Anesthesia. Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007; 116:1736–1754.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expanding transcatheter aortic valve replacement into uncharted indications
- Left Atrial Dissection by Aorto-Left Atrial Fistula after Aortic Valve Replacement: A case report
- Ruptured Subvalvular Aortic Aneurysm of a Person Who Has Bicuspid Aortic Valve
- Infective Endocarditis involving Aortic Valve, Mitral Valve, Tricuspid Valve, and Interventricular Septum: A Case Report
- A Case of Staphylococcal Tricuspid Valve Endocarditis With Para-Aortic Abscess in a Patient With Bicuspid Aortic Valve