J Cardiovasc Ultrasound.
2014 Sep;22(3):121-126. 10.4250/jcu.2014.22.3.121.
Myocardial Contrast Echocardiography for the Detection of Coronary Artery Disease in Patients with Global Hypokinesis Admitted for First-Onset Acute Heart Failure: Pilot Study
- Affiliations
-
- 1Cardiology Division, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. dgpark@hallym.or.kr
- 2Cardiology Division, KEPCO Medical Center, Seoul, Korea.
- KMID: 2045427
- DOI: http://doi.org/10.4250/jcu.2014.22.3.121
Abstract
- BACKGROUND
The non-invasive differentiation of ischemic and nonischemic acute heart failure (AHF) not resulting from acute myocardial infarction is difficult and has therapeutic and prognostic implications. The aim of this study was to assess whether resting myocardial contrast echocardiography (MCE) can detect coronary artery disease (CAD) in patients with decreased left ventricular (LV) systolic function and global hypokinesis presenting with AHF.
METHODS
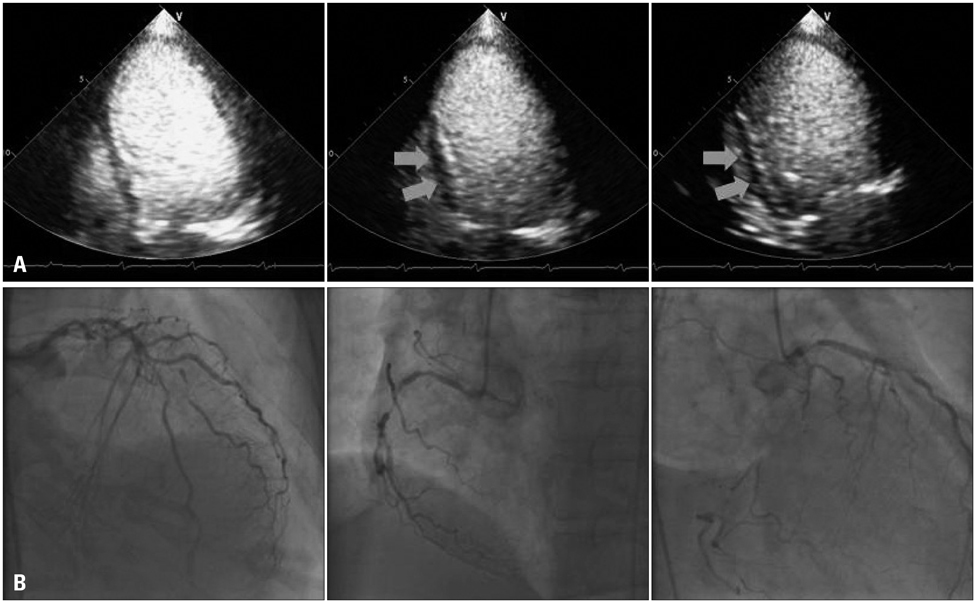
Twenty-one consecutive patients underwent low-power real-time MCE based on color-coded pulse inversion Doppler. Standard apical LV views were acquired during contrast IV infusion of Definity(R). Following transient microbubbles destruction, the contrast replenishment rate (beta), reflecting myocardial blood flow velocity, was derived by plotting signal intensity vs. time and fitting data to the exponential function: y (t) = A (1 - e(-beta(t-t0))) + C.
RESULTS
Of the 21 (mean age 56.6 +/- 13.6 years) patients, 5 (23.8%) demonstrated flow-limiting CAD (> 70% of luminal diameter narrowing). The mean +/- standard deviation of LV ejection fraction was 29.6 +/- 8.6%. Quantitative MCE analysis was feasible in 258 of 378 segments (68.3%). There were no significant difference in "beta" and "Abeta" in patients without and with CAD (0.48 +/- 0.27 vs. 0.45 +/- 0.25, p = 0.453 for beta and 2.99 +/- 2.23 vs. 3.68 +/- 3.13, p = 0.059 for Abeta, respectively). No contrast-related side effects were reported.
CONCLUSION
Resting quantitative MCE analysis in patients with AHF was feasible, however, the parameters did not aid in detecting of CAD.
Keyword
MeSH Terms
Figure
Reference
-
1. Gheorghiade M, Sopko G, De Luca L, Velazquez EJ, Parker JD, Binkley PF, Sadowski Z, Golba KS, Prior DL, Rouleau JL, Bonow RO. Navigating the crossroads of coronary artery disease and heart failure. Circulation. 2006; 114:1202–1213.
Article2. Fox KF, Cowie MR, Wood DA, Coats AJ, Gibbs JS, Underwood SR, Turner RM, Poole-Wilson PA, Davies SW, Sutton GC. Coronary artery disease as the cause of incident heart failure in the population. Eur Heart J. 2001; 22:228–236.
Article3. Bart BA, Shaw LK, McCants CB Jr, Fortin DF, Lee KL, Califf RM, O'Connor CM. Clinical determinants of mortality in patients with angiographically diagnosed ischemic or nonischemic cardiomyopathy. J Am Coll Cardiol. 1997; 30:1002–1008.
Article4. Purek L, Laule-Kilian K, Christ A, Klima T, Pfisterer ME, Perruchoud AP, Mueller C. Coronary artery disease and outcome in acute congestive heart failure. Heart. 2006; 92:598–602.
Article5. Flaherty JD, Rossi JS, Fonarow GC, Nunez E, Stough WG, Abraham WT, Albert NM, Greenberg BH, O'Connor CM, Yancy CW, Young JB, Davidson CJ, Gheorghiade M. Influence of coronary angiography on the utilization of therapies in patients with acute heart failure syndromes: findings from Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). Am Heart J. 2009; 157:1018–1025.
Article6. Follath F, Cleland JG, Klein W, Murphy R. Etiology and response to drug treatment in heart failure. J Am Coll Cardiol. 1998; 32:1167–1172.
Article7. Rossi JS, Flaherty JD, Fonarow GC, Nunez E, Gattis Stough W, Abraham WT, Albert NM, Greenberg BH, O'Connor CM, Yancy CW, Young JB, Davidson CJ, Gheorghiade M. Influence of coronary artery disease and coronary revascularization status on outcomes in patients with acute heart failure syndromes: a report from OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure). Eur J Heart Fail. 2008; 10:1215–1223.
Article8. Uretsky BF, Thygesen K, Armstrong PW, Cleland JG, Horowitz JD, Massie BM, Packer M, Poole-Wilson PA, Ryden L. Acute coronary findings at autopsy in heart failure patients with sudden death: results from the assessment of treatment with lisinopril and survival (ATLAS) trial. Circulation. 2000; 102:611–616.
Article9. Medina R, Panidis IP, Morganroth J, Kotler MN, Mintz GS. The value of echocardiographic regional wall motion abnormalities in detecting coronary artery disease in patients with or without a dilated left ventricle. Am Heart J. 1985; 109:799–803.
Article10. Chrysohoou C, Greenberg M, Stefanadis C. Non-invasive methods in differentiating ischaemic from non-ischaemic cardiomyopathy. A review paper. Acta Cardiol. 2006; 61:454–462.
Article11. Jeetley P, Hickman M, Kamp O, Lang RM, Thomas JD, Vannan MA, Vanoverschelde JL, van der Wouw PA, Senior R. Myocardial contrast echocardiography for the detection of coronary artery stenosis: a prospective multicenter study in comparison with single-photon emission computed tomography. J Am Coll Cardiol. 2006; 47:141–145.
Article12. Firschke C, Andrássy P, Linka AZ, Busch R, Martinoff S. Adenosine myocardial contrast echo in intermediate severity coronary stenoses: a prospective two-center study. Int J Cardiovasc Imaging. 2007; 23:311–321.
Article13. Senior R, Moreo A, Gaibazzi N, Agati L, Tiemann K, Shivalkar B, von Bardeleben S, Galiuto L, Lardoux H, Trocino G, Carrió I, Le Guludec D, Sambuceti G, Becher H, Colonna P, Ten Cate F, Bramucci E, Cohen A, Bezante G, Aggeli C, Kasprzak JD. Comparison of sulfur hexafluoride microbubble (SonoVue)-enhanced myocardial contrast echocardiography with gated single-photon emission computed tomography for detection of significant coronary artery disease: a large European multicenter study. J Am Coll Cardiol. 2013; 62:1353–1361.
Article14. Senior R, Janardhanan R, Jeetley P, Burden L. Myocardial contrast echocardiography for distinguishing ischemic from nonischemic first-onset acute heart failure: insights into the mechanism of acute heart failure. Circulation. 2005; 112:1587–1593.
Article15. Boff GM, Zanco P, Della Valentina P, Cardaioli P, Thiene G, Chioin R, Dalla Volta S. Positron emission tomography is a useful tool in differentiating idiopathic from ischemic dilated cardiomyopathy. Int J Cardiol. 2000; 74:67–74. discussion 75-6.
Article16. Malm S, Frigstad S, Helland F, Oye K, Slordahl S, Skjarpe T. Quantification of resting myocardial blood flow velocity in normal humans using real-time contrast echocardiography. A feasibility study. Cardiovasc Ultrasound. 2005; 3:16.
Article17. Wei K. Approaches to the detection of coronary artery disease using myocardial contrast echocardiography. Am J Cardiol. 2002; 90:48J–58J.
Article18. Abdelmoneim SS, Martinez MW, Mankad SV, Bernier M, Dhoble A, Pellikka PA, Chandrasekaran K, Oh JK, Mulvagh SL. Resting qualitative and quantitative myocardial contrast echocardiography to predict cardiac events in patients with acute myocardial infarction and percutaneous revascularization. Heart Vessels. 2014; [Epub ahead of print].
Article19. Jayaweera AR, Wei K, Coggins M, Bin JP, Goodman C, Kaul S. Role of capillaries in determining CBF reserve: new insights using myocardial contrast echocardiography. Am J Physiol. 1999; 277(6 Pt 2):H2363–H2372.20. Janardhanan R, Burden L, Senior R. Usefulness of myocardial contrast echocardiography in predicting collateral blood flow in the presence of a persistently occluded acute myocardial infarction-related coronary artery. Am J Cardiol. 2004; 93:1207–1211.
Article21. Kaul S. Myocardial contrast echocardiography: a 25-year retrospective. Circulation. 2008; 118:291–308.22. Watzinger N, Lund GK, Saeed M, Reddy GP, Araoz PA, Yang M, Schwartz AB, Bedigian M, Higgins CB. Myocardial blood flow in patients with dilated cardiomyopathy: quantitative assessment with velocity-encoded cine magnetic resonance imaging of the coronary sinus. J Magn Reson Imaging. 2005; 21:347–353.
Article23. Nitenberg A, Foult JM, Blanchet F, Zouioueche S. Multifactorial determinants of reduced coronary flow reserve after dipyridamole in dilated cardiomyopathy. Am J Cardiol. 1985; 55:748–754.
Article24. Abdelmoneim SS, Mankad SV, Bernier M, Dhoble A, Hagen ME, Ness SA, Chandrasekaran K, Pellikka PA, Oh JK, Mulvagh SL. Microvascular function in Takotsubo cardiomyopathy with contrast echocardiography: prospective evaluation and review of literature. J Am Soc Echocardiogr. 2009; 22:1249–1255.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Serial Echocardiograhic Obesrvation of Acute Myocardial Injury Associated with Pheoechromocytoma Crisis
- A Case of Acquired Coronary Artery Fistula to the Left Ventricle after Acute Myocardial Infarction
- Assessment of Myocardial Collateral Blood Flow with Contrast Echocardiography
- Coronary Artery Vasospasm
- Two Cases of Acute Myocardial Infarctions with Normal Coronary Arteriograms and Early Complete Recovery of Myocardial Dysfunction