J Korean Foot Ankle Soc.
2015 Sep;19(3):91-96. 10.14193/jkfas.2015.19.3.91.
When Do Clinical and Radiographic Results Stabilize after Proximal Chevron Osteotomy in Hallux Valgus?
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yeungnam University College of Medicine, Daegu, Korea. chpark77@naver.com
- 2Department of Orthopaedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2045011
- DOI: http://doi.org/10.14193/jkfas.2015.19.3.91
Abstract
- PURPOSE
The purpose of this study is to evaluate the sequential changes of clinical and radiographic results after proximal chevron osteotomy in patients with moderate to severe hallux valgus.
MATERIALS AND METHODS
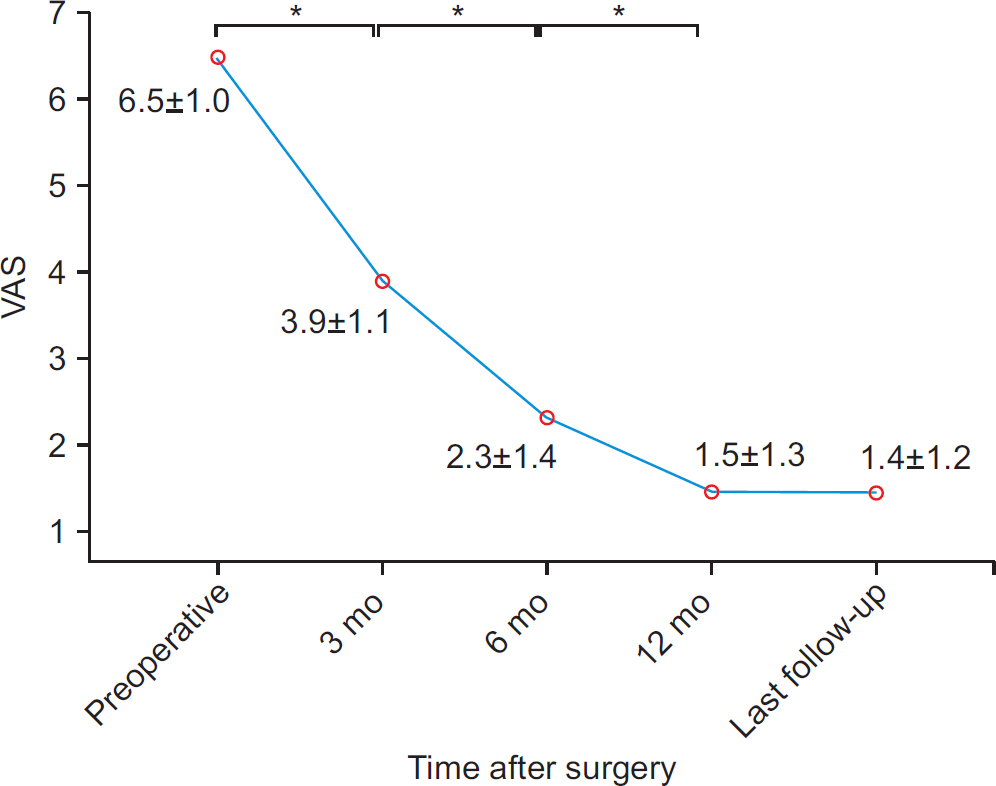
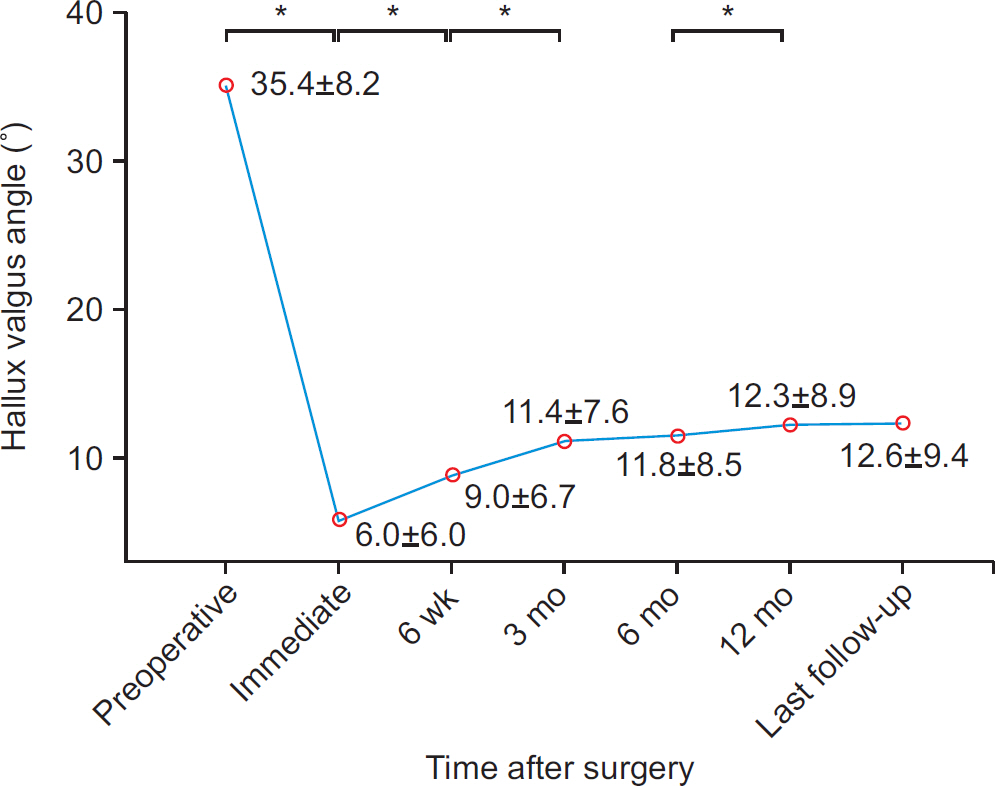
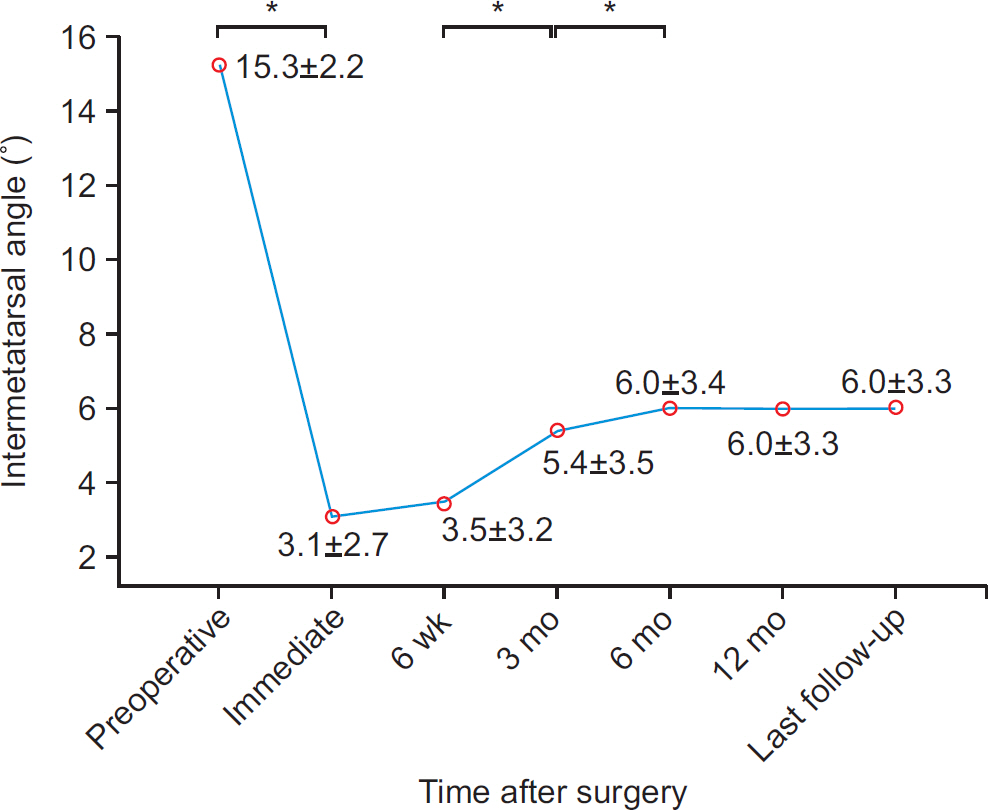
Between January 2008 and December 2009, 93 patients (117 feet) were treated with proximal chevron osteotomy and distal soft tissue procedure for symptomatic moderate to severe hallux valgus deformity. The mean age of patients was 51 years (range, 19 to 71) and the mean duration of follow-up was 27.5 months (range, 24 to 35). Clinical results were evaluated using visual analogue scale (VAS) and American Orthopaedic Foot and Ankle Society (AOFAS) score preoperatively, at 3, 6, and 12 months after surgery, and at the last follow-up. Radiographic parameters including hallux valgus angle, intermetatarsal angle, and sesamoid position were evaluated preoperatively, immediately postoperatively, at 6 weeks, at 3, 6, and 12 months after surgery, and at the last follow-up.
RESULTS
VAS and AOFAS score showed significant improvement until 12 months after surgery. Hallux valgus angle and sesamoid position stabilized at 12 months after surgery and intermetatarsal angle stabilized at 6 months after surgery.
CONCLUSION
Clinical and radiographic results were stabilized beyond 12 months after proximal chevron osteotomy in patients with moderate to severe hallux valgus.
Figure
Reference
-
References
1. Coughlin MJ, Jones CP. Hallux valgus and first ray mobility. A prospective study. J Bone Joint Surg Am. 2007; 89:1887–98.2. Lee WC, Kim YM. Correction of hallux valgus using lateral soft-tissue release and proximal Chevron osteotomy through a medial incision J Bone Joint Surg Am. 2007; 89(Suppl 3):82–9.3. Mann RA, Rudicel S, Graves SC. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A longterm follow-up. J Bone Joint Surg Am. 1992; 74:124–9.
Article4. Park CH, Jang JH, Lee SH, Lee WC. A comparison of proximal and distal chevron osteotomy for the correction of moderate hallux valgus deformity. Bone Joint J. 2013; 95-B:649–56.
Article5. Easley ME, Kiebzak GM, Davis WH, Anderson RB. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int. 1996; 17:307–16.
Article6. Zettl R, Trnka HJ, Easley M, Salzer M, Ritschl P. Moderate to severe hallux valgus deformity: correction with proximal crescentic osteotomy and distal soft-tissue release. Arch Orthop Trauma Surg. 2000; 120:397–402.
Article7. Park CH, Lee WC, Kim JR, Lim SW. Characteristics of severe hallux valgus deformity with moderate intermetatarsal angle. J Korean Foot Ankle Soc. 2014; 18:173–7.
Article8. Kim TS, Kim HJ, Park YH, Lim HT. The differences of fixation method in proximal chevron osteotomy for hallux valgus: K-Wire, cannulated screw, plate. J Korean Foot Ankle Soc. 2011; 15:62–7.9. Gallentine JW, Deorio JK, Deorio MJ. Bunion surgery using locking-plate fixation of proximal metatarsal chevron osteotomies. Foot Ankle Int. 2007; 28:361–8.
Article10. Veri JP, Pirani SP, Claridge R. Crescentic proximal metatarsal osteotomy for moderate to severe hallux valgus: a mean 1212 year follow-up study. Foot Ankle Int. 2001; 22:817–22.11. Thordarson DB, Leventen EO. Hallux valgus correction with proximal metatarsal osteotomy: two-year follow-up. Foot Ankle. 1992; 13:321–6.
Article12. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Shima H. Proximal metatarsal osteotomy for hallux valgus: comparison of outcome for moderate and severe deformities. Foot Ankle Int. 2008; 29:664–70.
Article13. Tanaka Y, Takakura Y, Kumai T, Sugimoto K, Taniguchi A, Hattori K. Proximal spherical metatarsal osteotomy for the foot with severe hallux valgus. Foot Ankle Int. 2008; 29:1025–30.
Article14. Okuda R, Kinoshita M, Morikawa J, Yasuda T, Abe M. Proximal metatarsal osteotomy: relation between 1- to greater than 3-years results. Clin Orthop Relat Res. 2005; 435:191–6.15. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994; 15:349–53.
Article16. Hardy RH, Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951; 33-B:376–91.17. Schneider W, Knahr K. Surgery for hallux valgus. The expectations of patients and surgeons Int Orthop. 2001; 25:382–5.18. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009; 91:1637–45.
Article19. Bonnel F, Canovas F, Poirée G, Dusserre F, Vergnes C. Evaluation of the Scarf osteotomy in hallux valgus related to distal metatarsal articular angle: a prospective study of 79 operated cases1 Rev Chir Orthop Reparatrice Appar Mot1. 1999; 85:381–61.20. Deenik AR, de Visser E, Louwerens JW, de Waal Malefijt M, Drai-jer FF, de Bie RA. Hallux valgus angle as main predictor for correction of hallux valgus1 BMC Musculoskelet Disord1. 2008; 9:70.21. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2007; 89:2163–72.
Article22. Pontious J, Mahan KT, Carter S. Characteristics of adolescent hallux abducto valgus. A retrospective review. J Am Podiatr Med Assoc. 1994; 84:208–18.
Article23. Crosby LA, Bozarth GR. Fixation comparison for chevron osteotomies. Foot Ankle Int. 1998; 19:41–3.
Article24. Chow FY, Lui TH, Kwok KW, Chow YY. Plate fixation for crescentic metatarsal osteotomy in the treatment of hallux valgus: an eight-year followup study. Foot Ankle Int. 2008; 29:29–33.
Article25. Klos K, Gueorguiev B, Mückley T, Fröber R, Hofmann GO, Schwieger K, et al. Stability of medial locking plate and compression screw versus two crossed screws for lapidus arthrodesis. Foot Ankle Int. 2010; 31:158–63.26. Varner KE, Matt V, Alexander JW, Johnston JD, Younas S, Mary-mont JV, et al. Screw versus plate fixation of proximal first metatarsal crescentic osteotomy. Foot Ankle Int. 2009; 30:142–9.
Article27. Park CH, Ahn JY, Kim YM, Lee WC. Plate fixation for proximal chevron osteotomy has greater risk for hallux valgus recurrence than Kirschner wire fixation. Int Orthop. 2013; 37:1085–92.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chevron Osteotomy as the Treatment of Moderate to Severe Hallux Valgus Deformity
- Treatment of Severe Hallux Valgus Deformity with Proximal Reverse Chevron Metatarsal Osteotomy and Akin Osteotomy
- A Comparison of Operative Treatment of Hallux Valgus with a Proximal Metatarsal Osteotomy and with a Modified Chevron Osteotomy
- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
- Comparison of the Results between Distal Chevron Osteotomy and Proximal Metatarsal Osteotomy for the Treatment of Moderate Hallux Valgus