J Korean Fract Soc.
2015 Apr;28(2):132-138. 10.12671/jkfs.2015.28.2.132.
Progression of Compression and Related Factors in Conservative Management of Osteoporotic Vertebral Compression Fractures
- Affiliations
-
- 1Department of Orthopaedic Surgery, Ewha Womans University School of Medicine, Seoul, Korea. ydkoh@ewha.ac.kr
- KMID: 2044021
- DOI: http://doi.org/10.12671/jkfs.2015.28.2.132
Abstract
- PURPOSE
The purpose of this study is to determine the ideal period of brace application for thoracolumbar (T10-L2) osteoporotic vertebral compression fracture (OVCF) based on the progression of the vertebral compression with passage of time and to evaluate the factors associated with progression of thoracolumbar OVCF, when treated conservatively.
MATERIALS AND METHODS
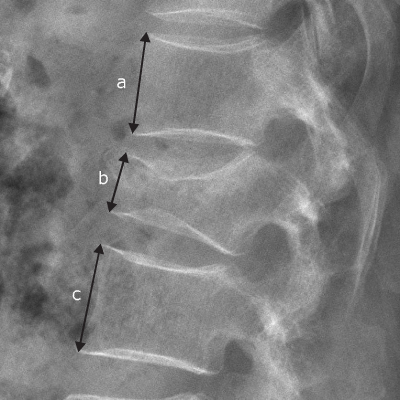
This retrospective study included a total of 46 patients who were diagnosed with thoracolumbar OVCF and could be followed-up for at least 6 months. In this study, the increase of compression rate and the mean slope of compression rate per weeks were compared between two periods (from diagnosed date to 8 weeks and from 8 weeks to 6 months), as the standard point. Age, bone mineral density (BMD), osteoporosis treatment after injury, diabetes mellitus (DM) as underlying disease were also compared between two groups (setting up 15% as standard point of increase of compression rate, <15% and > or =15%). Statistical analyses were performed using the paired t-test to assess the increase of compression rate and using the linear mixed model to assess the mean slope change. The relationships between the factors and progression of compression were analyzed using t-test, chi-square test, and logistic regression analysis.
RESULTS
The increase of compression rate was 13.03% and 1.97% in each period and the difference between those two periods was 11.06% (p=0.00). At 8 weeks of follow-up, the mean slope was reduced by 1.12 (p=0.00). No statistically significant difference in related factors was observed between two groups.
CONCLUSION
Considering the increase of compression rate with passage of time, brace should be applied strictly for an initial 8 weeks. And age, BMD, osteoporosis treatment after injury, and DM as underlying disease are not predictors of progression of compression in vertebral fractures.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Influence of Initial Magnetic Resonance Imaging Findings on the Compression Rate of Thoracolumbar Osteoporotic Vertebral Compression Fracture
Seok-Ha Hwang, Seung-Pyo Suh, Young-Kyun Woo, Ho-Seung Jeon, Ho-Won Jeong
J Korean Orthop Assoc. 2018;53(4):341-349. doi: 10.4055/jkoa.2018.53.4.341.Treatment Effect with Weekly Teriparatide in the Vertebral Compression Fractures in Patients with Severe Osteoporosis
Seok-Ha Hwang, Young-Kyun Woo, Ho-Seung Jeon, Seung-Pyo Suh, Joo-Young Kim, Jae-Nam Kim
J Korean Orthop Assoc. 2019;54(6):528-536. doi: 10.4055/jkoa.2019.54.6.528.
Reference
-
1. Borgström F, Zethraeus N, Johnell O, et al. Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int. 2006; 17:637–650.
Article2. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17:1726–1733.
Article3. Hasserius R, Karlsson MK, Jónsson B, Redlund-Johnell I, Johnell O. Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly: a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int. 2005; 76:235–242.
Article4. Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O. –European Vertebral Osteoporosis Study. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003; 14:61–68.
Article5. Klazen CA, Verhaar HJ, Lampmann LE, et al. VERTOS II: percutaneous vertebroplasty versus conservative therapy in patients with painful osteoporotic vertebral compression fractures; rationale, objectives and design of a multicenter randomized controlled trial. Trials. 2007; 8:33.
Article6. Boonen S, Wahl DA, Nauroy L, et al. Balloon kyphoplasty and vertebroplasty in the management of vertebral compression fractures. Osteoporos Int. 2011; 22:2915–2934.
Article7. Ha KY, Lee JS, Kim KW, Chon JS. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br. 2006; 88:629–633.
Article8. Prather H, Watson JO, Gilula LA. Nonoperative management of osteoporotic vertebral compression fractures. Injury. 2007; 38:Suppl 3. S40–S48.
Article9. Longo UG, Denaro L, Campi S, Maffulli N, Denaro V. Upper cervical spine injuries: indications and limits of the conservative management in Halo vest A systematic review of efficacy and safety. Injury. 2010; 41:1127–1135.
Article10. Park JH, Kang KC, Shin DE, Koh YG, Son JS, Kim BH. Preventive effects of conservative treatment with short-term teriparatide on the progression of vertebral body collapse after osteoporotic vertebral compression fracture. Osteoporos Int. 2014; 25:613–618.
Article11. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006; 6:479–487.
Article12. Dewar C. Diagnosis and treatment of vertebral compression fractures. Radiol Technol. 2015; 86:301–320. quiz 321-323.13. Chang V, Holly LT. Bracing for thoracolumbar fractures. Neurosurg Focus. 2014; 37:E3.
Article14. Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone. 1996; 18:185S–189S.
Article15. Crans GG, Silverman SL, Genant HK, Glass EV, Krege JH. Association of severe vertebral fractures with reduced quality of life: reduction in the incidence of severe vertebral fractures by teriparatide. Arthritis Rheum. 2004; 50:4028–4034.
Article16. Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ 3rd. Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993; 137:1001–1005.
Article17. Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004; 83:177–186.
Article18. Ha KY, Kim YH. Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos Int. 2013; 24:1207–1213.
Article19. Sohn JM, Kim KW, Ha KY, Ha NK, Kim YH, Kim JH. Risk factors for the progressive osteoporotic spinal fracture. J Korean Soc Spine Surg. 2009; 16:153–159.
Article20. Kim JH, Seo JG, Ahn JH. Correlation between progression of compression and bone densiometry index in osteoporotic compression fracture of thoracolumbar spine. J Korean Fract Soc. 2006; 19:254–258.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- Comparison of the Result of Vertebroplasty and Conservative Treatment in Osteoporotic Vertebral Compression Fracture
- Clinical Outcome of Conservative Treatment for Osteoporotic Compression Fractures in Thoracolumbar Junction
- Correlation between Progression of Compression and Bone Densiometry Index in Osteoporotic Compression Fracture of Thoracolumbar Spine
- Treatment Options of Osteoporotic Vertebral Compression Fractures