J Korean Soc Radiol.
2014 Apr;70(4):291-294. 10.3348/jksr.2014.70.4.291.
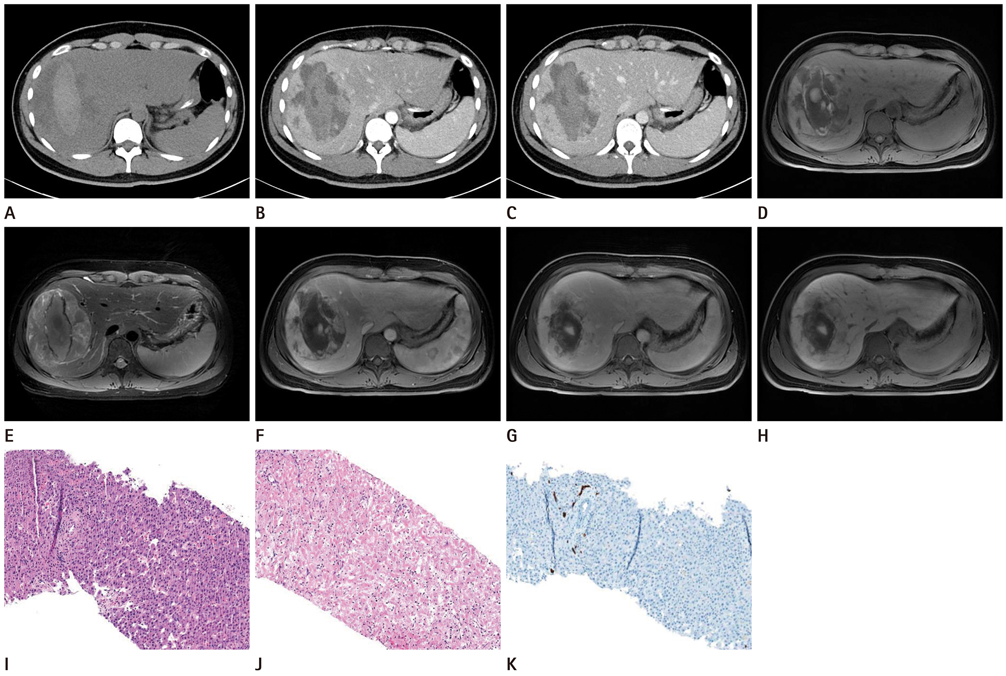
Hemorrhagic Focal Nodular Hyperplasia in Young Men: A Case Report
- Affiliations
-
- 1Department of Diagnostic Radiology, College of Medicine, Dong-A University, Busan, Korea. risual@dau.ac.kr
- 2Department of Surgery, College of Medicine, Dong-A University, Busan, Korea.
- 3Department of Pathology, College of Medicine, Dong-A University, Busan, Korea.
- KMID: 2041940
- DOI: http://doi.org/10.3348/jksr.2014.70.4.291
Abstract
- In general, focal nodular hyperplasia is a hepatic lesion that most frequently affects the healthy women of reproductive age. Focal nodular hyperplasia lesions have a benign natural course; the majority of the cases remain asymptomatic and complications are rare. Spontaneous hemorrhage of focal nodular hyperplasia is a rare disease, and the hemorrhage in young men is even more uncommon. We report a rare case of spontaneous hemorrhage of focal nodular hyperplasia in a 19-year-old man.
MeSH Terms
Figure
Reference
-
1. Casillas VJ, Amendola MA, Gascue A, Pinnar N, Levi JU, Perez JM. Imaging of nontraumatic hemorrhagic hepatic lesions. Radiographics. 2000; 20:367–378.2. Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am. 1975; 59:995–1013.3. Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985; 5:1194–1200.4. Li T, Qin LX, Ji Y, Sun HC, Ye QH, Wang L, et al. Atypical hepatic focal nodular hyperplasia presenting as acute abdomen and misdiagnosed as hepatocellular carcinoma. Hepatol Res. 2007; 37:1100–1105.5. Becker YT, Raiford DS, Webb L, Wright JK, Chapman WC, Pinson CW. Rupture and hemorrhage of hepatic focal nodular hyperplasia. Am Surg. 1995; 61:210–214.6. Knowles DM 2nd, Casarella WJ, Johnson PM, Wolff M. The clinical, radiologic, and pathologic characterization of benign hepatic neoplasms Alleged association with oral contraceptives. Medicine (Baltimore). 1978; 57:223–237.7. Whelan TJ Jr, Baugh JH, Chandor S. Focal nodular hyperplasia of the liver. Ann Surg. 1973; 177:150–158.8. Goodwin MD, Dobson JE, Sirlin CB, Lim BG, Stella DL. Diagnostic challenges and pitfalls in MR imaging with hepatocyte-specific contrast agents. Radiographics. 2011; 31:1547–1568.9. Scalori A, Tavani A, Gallus S, La Vecchia C, Colombo M. Risk factors for focal nodular hyperplasia of the liver: an Italian case-control study. Am J Gastroenterol. 2002; 97:2371–2373.10. Mathieu D, Kobeiter H, Maison P, Rahmouni A, Cherqui D, Zafrani ES, et al. Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology. 2000; 118:560–564.