Korean J Obstet Gynecol.
2010 Dec;53(12):1085-1091. 10.5468/kjog.2010.53.12.1085.
Decrease in acceptance of genetic amniocentesis after alteration of social conditions toward pregnancy termination
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea. bjkimmd7@snu.ac.kr
- KMID: 2037509
- DOI: http://doi.org/10.5468/kjog.2010.53.12.1085
Abstract
OBJECTIVE
To investigate the effect of alteration of social conditions towards pregnancy termination on the acceptance of genetic amniocentesis.
METHODS
Retrospective review of medical records was conducted for women (<20 weeks' gestation, singleton pregnancy) who visited our outpatient department between February 1, 2009 and August 31, 2010. Acceptance of genetic amniocentesis was compared between two groups of women: one from February 1, 2009 to November 30, 2009 (2009 group) and the other from December 1, 2009 to August 31, 2010 (2010 group) after strict regulation of pregnancy termination. The acceptance rate of those who were referred to our center for genetic amniocentesis in same time period was also evaluated.
RESULTS
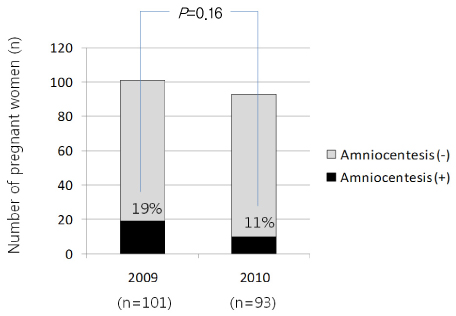
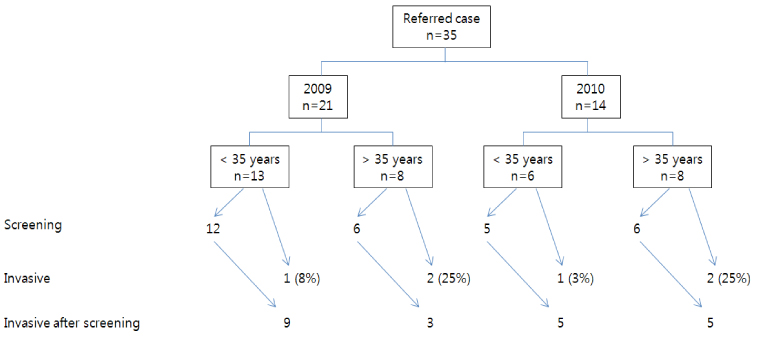
Overall, 19 of 101 (19%) women in the 2009 group and 10 of 93 (11%) in the 2010 group, opted for invasive diagnostic methods (P=0.16). Women > 35 years in the 2010 group (5/30, 17%) were less likely to accept genetic amniocentesis than 2009 group (15/30, 50%; P=0.01). Similar results were observed in those who were indicated for genetic amniocentesis. (9/35, 26% vs 19/34, 56%; P=0.02). Acceptance rate of genetic amniocentesis was increased for those who were referred from private clinic, but without statistical significance (15/21, 71% vs 13/14, 93%; P=0.20).
CONCLUSION
After strict regulation of pregnancy termination, acceptance rate of genetic amniocentesis was significantly decreased among women who had increased risk for chromosomal abnormalities or neural tube defect at our center. Whereas, there were no significant change in acceptance rate for those who were referred for amniocentesis from private clinic.
MeSH Terms
Figure
Reference
-
1. Elimian A, Demsky M, Figueroa R, Ogburn P, Spitzer AR, Gerald Quirk J. The influence of IVF, multiple gestation and miscarriage on the acceptance of genetic amniocentesis. Prenat Diagn. 2003. 23:501–503.2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 27: Clinical Management Guidelines for Obstetrician-Gynecologists. Prenatal diagnosis of fetal chromosomal abnormalities. Obstet Gynecol. 2001. 97(5Pt1):suppl 1–suppl 12.3. Kim HM. The necessity and direction of revising article 14 of the mother and child health law. Korean J Obstet Gynecol. 2009. 52:487–498.4. Son YS. The medicolegal understanding regarding fetocide in the criminal law and artificial termination in the mother and child health law. Korean J Obstet Gynecol. 2010. 53:467–474.5. Chae YH, Seo K, Yoon DK, Oh JR, Lee MB, Lee KE. A research on the actual condition of antenatal screening application in obstetric clinics in Korea and suggestions for preparation of antenatal screening guideline. Korean J Obstet Gynecol. 2006. 49:55–63.6. Park IY, Shin JC, Kim SC, Ahn HY, Moon HB, Park CH, et al. Cytogenetic analysis in 3,503 cases of midtrimester smniocentesis: CUMC experience (II). Korean J Obstet Gynecol. 2004. 47:96–103.7. Chun YY, Ku JY, Song JW, Kim BS, Bae YY, Sun JG, et al. Clinical analysis of 739 cases of midtrimester amniocentesis. Korean J Perinatol. 2005. 16:146–153.8. Jang SK, Choi OH. Cytogenetic and clinical analysis in 3,537 cases of midtrimester smniocentesis. Korean J Perinatol. 2007. 18:29–36.9. Shim JY, Kim SH, Kim JS, Ahn SM, Seo EJ, Yoo HW, et al. Clinical snalysis of prenatal cytogenetic diagnoses: four-year experience at Asan Medical Center. Korean J Obstet Gynecol. 2004. 47:487–494.10. Kim KM, Cho JY, Park MH, Kim SH, Kim BJ. Matermal serum screening test for fetal Down syndrome. Korean J Obstet Gynecol. 1998. 41:2593–2598.11. Choi YK, Kim MY, Han JY, Ryu HM, Yang JH, Kim ES, et al. A Study about the effect iveness of triple marker test as a screening test for chromosomal aneuploidy. Korean J Obstet Gynecol. 1999. 42:1935–1942.12. Green JM, Hewison J, Bekker HL, Bryant LD, Cuckle HS. Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review. Health Technol Assess. 2004. 8:iii, ix-x, 1-109.13. Kuppermann M, Learman LA, Gates E, Gregorich SE, Nease RF Jr, Lewis J, et al. Beyond race or ethnicity and socioeconomic status: predictors of prenatal testing for Down syndrome. Obstet Gynecol. 2006. 107:1087–1097.14. Garcia E, Timmermans DR, van Leeuwen E. The impact of ethical beliefs on decisions about prenatal screening tests: searching for justification. Soc Sci Med. 2008. 66:753–764.15. Kelly SE. Choosing not to choose: reproductive responses of parents of children with genetic conditions or impairments. Sociol Health Illn. 2009. 31:81–97.16. Markens S, Browner CH, Press N. 'Because of the risks': how US pregnant women account for refusing prenatal screening. Soc Sci Med. 1999. 49:359–369.17. Viljoen D, Oosthuizen C, van der Westhuizen S. Patient attitudes to prenatal screening and termination of pregnancy at Groote Schuur Hospital: a two year prospective study. East Afr Med J. 1996. 73:327–329.18. Elimian A, Demsky M, Figueroa R, Ogburn P, Spitzer AR, Quirk JG. The influence of genetic counselors on the acceptance of mid-trimester amniocentesis. J Matern Fetal Neonatal Med. 2005. 17:219–221.19. Saucier JB, Johnston D, Wicklund CA, Robbins-Furman P, Hecht JT, Monga M. Racial-ethnic differences in genetic amniocentesis uptake. J Genet Couns. 2005. 14:189–195.20. Usta IM, Nassar AH, Abu-Musa AA, Hannoun A. Effect of religion on the attitude of primiparous women toward genetic testing. Prenat Diagn. 2010. 30:241–246.21. Sharda S, Phadke SR. Uptake of invasive prenatal diagnostic tests in women after detection of soft markers for chromosomal abnormality on ultrasonographic evaluation. J Perinatol. 2007. 27:550–555.22. Wray AM, Ghidini A, Alvis C, Hodor J, Landy HJ, Poggi SH. The impact of first-trimester screening on AMA patients' uptake of invasive testing. Prenat Diagn. 2005. 25:350–353.23. Zoppi MA, Ibba RM, Putzolu M, Floris M, Monni G. Nuchal translucency and the acceptance of invasive prenatal chromosomal diagnosis in women aged 35 and older. Obstet Gynecol. 2001. 97:916–920.24. Nakata N, Wang Y, Bhatt S. Trends in prenatal screening and diagnostic testing among women referred for advanced maternal age. Prenat Diagn. 2010. 30:198–206.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetic amniocentesis after multifetal pregnancy reduction
- A Case of Prenatal Diagnosis of 47, XXY Klinehelter Syndrome
- Second trimester selective termination in a dizygotic twin pregnancy with discordancy for Down's syndrome: A case report
- Prenatal Diagnosis with Genetic Amniocentesis
- A Study on Genetic Amniocentesis in Pregnant Women