J Gynecol Oncol.
2010 Jun;21(2):87-92. 10.3802/jgo.2010.21.2.87.
Absence of dysplasia in the excised cervix by a loop electrosurgical excision procedure in the treatment of cervical intraepithelial neoplasia
- Affiliations
-
- 1Department of Obstetrics & Gynecology, Soonchunhyang University Hospital, Bucheon, Korea. khnambc@yahoo.co.kr
- 2Department of Pathology, Soonchunhyang University Hospital, Bucheon, Korea.
- KMID: 2009576
- DOI: http://doi.org/10.3802/jgo.2010.21.2.87
Abstract
OBJECTIVE
Absence of dysplasia in the excised specimen following loop electrosurgical excision procedure (LEEP) for treatment of cervical intraepithelial neoplasia (CIN) 2/3 is an occasional finding of uncertain clinical significance. We evaluated several factors including age, liquid-based Pap (LBP) test, human papillomavirus (HPV) load before treatment, and HPV typing as predictors for absence of dysplasia. Absence of dysplasia in LEEP specimens was analyzed in terms of factors for recurrent disease after LEEP conization
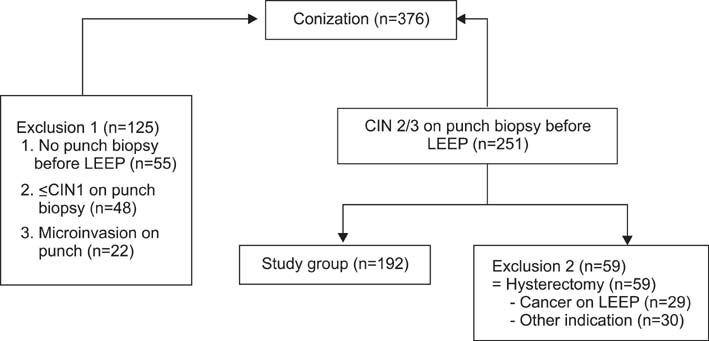
METHODS
In total, 192 women (mean age, 39.3+/-8.4 years; range, 24 to 70 years) with biopsy-proven CIN 2/3 were treated by LEEP conization. Age, LBP test, histological grade, HPV load, and HPV DNA typing were evaluated as possible predictors of the absence of residual dysplasia or recurrent disease.
RESULTS
Of the LEEP specimens, 34 (17.7%) showed no dysplasia in preoperative biopsies from patients with proven CIN 2/3. Low HPV load (<100 relative light units [RLU]) was significantly related to the absence of dysplasia in LEEP specimens, using logistic regression. Margin involvement and high HPV load (> or =400 RLU) were significant factors for recurrence.
CONCLUSION
Absence of dysplasia in LEEP specimens occurred in 17.7% of our specimens. Prediction of the absence of dysplasia in LEEP specimens was associated with low HPV load. Residual/recurrent disease after LEEP was associated with a positive resection margin and high viral load, and was not associated with absence of dysplasia in LEEP specimens. Even if there is no dysplasia in conization specimens, close follow-up for residual/recurrent disease is needed.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical factors that affect diagnostic discrepancy between colposcopically directed biopsies and loop electrosurgical excision procedure conization of the uterine cervix
Yuyeon Jung, Ah Ra Lee, Sung-Jong Lee, Yong Seok Lee, Dong Choon Park, Eun Kyung Park
Obstet Gynecol Sci. 2018;61(4):477-488. doi: 10.5468/ogs.2018.61.4.477.
Reference
-
1. Lee HB, Lee YS, Lee KH, Kim CJ, Park JS. A case of advanced gynecologic pelvic tumors showing the diagnostic utility of HPV analysis. J Gynecol Oncol. 2009. 20:251–253.2. Snijders PJ, Hogewoning CJ, Hesselink AT, Berkhof J, Voorhorst FJ, Bleeker MC, et al. Determination of viral load thresholds in cervical scrapings to rule out CIN 3 in HPV 16, 18, 31 and 33-positive women with normal cytology. Int J Cancer. 2006. 119:1102–1107.3. Park JS, Hwang ES, Park SN, Ahn HK, Um SJ, Kim CJ, et al. Physical status and expression of HPV genes in cervical cancers. Gynecol Oncol. 1997. 65:121–129.4. Wright TC Jr, Cox JT, Massad LS, Twiggs LB, Wilkinson EJ. 2001 Consensus Guidelines for the management of women with cervical cytological abnormalities. JAMA. 2002. 287:2120–2129.5. Eduardo AM, Dinh TV, Hannigan EV, Yandell RB, Schnadig VJ. Outpatient loop electrosurgical excision procedure for cervical intraepithelial neoplasia: can it replace cold knife conization? J Reprod Med. 1996. 41:729–732.6. Brockmeyer AD, Wright JD, Gao F, Powell MA. Persistent and recurrent cervical dysplasia after loop electrosurgical excision procedure. Am J Obstet Gynecol. 2005. 192:1379–1381.7. Alonso I, Torne A, Puig-Tintore LM, Esteve R, Quinto L, Campo E, et al. Pre- and post-conization high-risk HPV testing predicts residual/recurrent disease in patients treated for CIN 2-3. Gynecol Oncol. 2006. 103:631–636.8. Clavel C, Cucherousset J, Lorenzato M, Caudroy S, Nou JM, Nazeyrollas P, et al. Negative human papillomavirus testing in normal smears selects a population at low risk for developing high-grade cervical lesions. Br J Cancer. 2004. 90:1803–1808.9. Pinto AP, Crum CP. Natural history of cervical neoplasia: defining progression and its consequence. Clin Obstet Gynecol. 2000. 43:352–362.10. Prendiville W, Cullimore J, Norman S. Large loop excision of the transformation zone (LLETZ): a new method of management for women with cervical intraepithelial neoplasia. Br J Obstet Gynaecol. 1989. 96:1054–1060.11. Li ZG, Qian de Y, Cen JM, Chen GD, Shu YH. Three-step versus "see-and-treat" approach in women with high-grade squamous intraepithelial lesions in a low-resource country. Int J Gynaecol Obstet. 2009. 106:202–205.12. Sherman ME, Wang SS, Tarone R, Rich L, Schiffman M. Histopathologic extent of cervical intraepithelial neoplasia 3 lesions in the atypical squamous cells of undetermined significance low-grade squamous intraepithelial lesion triage study: implications for subject safety and lead-time bias. Cancer Epidemiol Biomarkers Prev. 2003. 12:372–379.13. Berdichevsky L, Karmin R, Chuang L. Treatment of high-grade squamous intraepithelial lesions: a 2- versus 3-step approach. Am J Obstet Gynecol. 2004. 190:1424–1426.14. Kinney SR, Cohn AR. Predicting "no residual dysplasia" in loop electrosurgical exision specimens. 2006 Biennial Meeting of ASCCP. J Low Genit Tract Dis. 2006. 10:173.15. Husseinzadeh N, Shbaro I, Wesseler T. Predictive value of cone margins and post-cone endocervical curettage with residual disease in subsequent hysterectomy. Gynecol Oncol. 1989. 33:198–200.16. Phelps JY 3rd, Ward JA, Szigeti J 2nd, Bowland CH, Mayer AR. Cervical cone margins as a predictor for residual dysplasia in post-cone hysterectomy specimens. Obstet Gynecol. 1994. 84:128–130.17. Soutter WP, de Barros Lopes A, Fletcher A, Monaghan JM, Duncan ID, Paraskevaidis E, et al. Invasive cervical cancer after conservative therapy for cervical intraepithelial neoplasia. Lancet. 1997. 349:978–980.18. Paraskevaidis E, Kalantaridou SN, Paschopoulos M, Zikopoulos K, Diakomanolis E, Dalkalitsis N, et al. Factors affecting outcome after incomplete excision of cervical intraepithelial neoplasia. Eur J Gynaecol Oncol. 2003. 24:541–543.19. Nagai Y, Maehama T, Asato T, Kanazawa K. Persistence of human papillomavirus infection after therapeutic conization for CIN 3: is it an alarm for disease recurrence? Gynecol Oncol. 2000. 79:294–299.20. Costa S, De Simone P, Venturoli S, Cricca M, Zerbini ML, Musiani M, et al. Factors predicting human papillomavirus clearance in cervical intraepithelial neoplasia lesions treated by conization. Gynecol Oncol. 2003. 90:358–365.21. Moore BC, Higgins RV, Laurent SL, Marroum MC, Bellitt P. Predictive factors from cold knife conization for residual cervical intraepithelial neoplasia in subsequent hysterectomy. Am J Obstet Gynecol. 1995. 173:361–366.22. Park JY, Bae J, Lim MC, Lim SY, Lee DO, Kang S, et al. Role of high risk-human papilloma virus test in the follow-up of patients who underwent conization of the cervix for cervical intraepithelial neoplasia. J Gynecol Oncol. 2009. 20:86–90.23. Nam K, Chung S, Kim J, Jeon S, Bae D. Factors associated with HPV persistence after conization in patients with negative margins. J Gynecol Oncol. 2009. 20:91–95.24. Gok M, Coupe VM, Berkhof J, Verheijen RH, Helmerhorst TJ, Hogewoning CJ, et al. HPV16 and increased risk of recurrence after treatment for CIN. Gynecol Oncol. 2007. 104:273–275.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Concepts of Cervical Conization
- Hemoperitoneum: a complication of loop electrosurgical excision procedure
- Treatment of the patients with abnormal cervical cytology: a "see-and-treat" versus three-step strategy
- The accuracy of cervical cancer and cervical intraepithelial neoplasia diagnosis with loop electrosurgical excisional procedure under colposcopic vision
- F-18 FDG PET Images of the Cervix at Various Time Points after the Loop Electrosurgical Excision Procedure