J Korean Soc Radiol.
2011 Oct;65(4):389-394. 10.3348/jksr.2011.65.4.389.
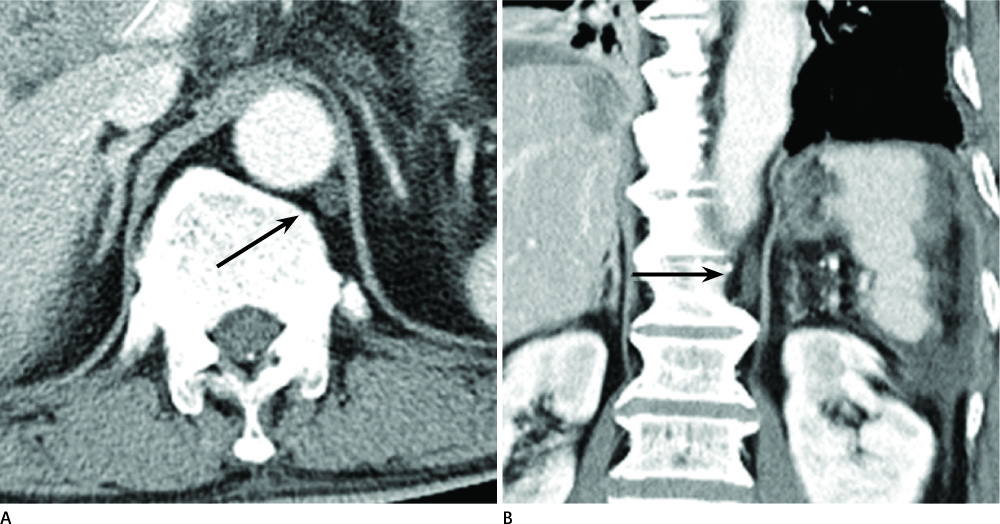
The Cisterna Chyli in Gastrointestinal Malignancy Patients: Incidence and Finding in CT
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University College of Medicine, Bucheon, Korea. hklee@schmc.ac.kr
- 2Department of Radiology, Kyung Hee University College of Medicine, Seoul, Korea.
- KMID: 2002940
- DOI: http://doi.org/10.3348/jksr.2011.65.4.389
Abstract
- PURPOSE
To evaluate the incidence and volume of the cisterna chyli of gastrointestinal malignancy patients by CT.
MATERIALS AND METHODS
Contrast enhanced abdominal CT images of gastrointestinal malignancies from 1,421 patients were evaluated. The prevalence of cisterna chyli according to origin of primary tumor was recorded, and the volume of identifiable cisterna chyli was calculated. The average volumes were then compared by the ANOVA method.
RESULTS
The cisterna chyli was found in 352 patients (25.1%). Of these, the incidences by location were hepatocelluar carcinoma, 33.6% (n = 82), biliary carcinoma, 24.6% (n = 42), colon cancer 24.1% (n = 84), pancreatic cancer, 23.6% (n = 17), and gastric cancer, 22.4% (n = 127). The average volume of cisterna chyli was 387 microL, which was calculated from the averages by location as follows: biliary carcinoma 567 microL, colon cancer 536 microL, hepatocellular carcinoma 360 microL, gastric cancer 275 microL, and pancreas cancer 178 microL. No significant difference was found among primary tumors.
CONCLUSION
Knowing the characteristics of the cisterna chyli is important for differentiating them from metastatic lymph nodes. The cisterna chyli of gastrointestinal malignancies was most commonly found in hepatocellular carcinoma cases. Further, no statistical difference among the volumes of the cisterna chyli or the origin of the primary tumors.
MeSH Terms
Figure
Reference
-
1. Feuerlein S, Kreuzer G, Schmidt SA, Muche R, Juchems MS, Aschoff AJ, et al. The cisterna chyli: prevalence, characteristics and predisposing factors. Eur Radiol. 2009; 19:73–78.2. Smith TR, Grigoropoulos J. The cisterna chyli: incidence and characteristics on CT. Clin Imaging. 2002; 26:18–22.3. Gollub MJ, Castellino RA. The cisterna chyli: a potential mimic of retrocrural lymphadenopathy on CT scans. Radiology. 1996; 199:477–480.4. Schoellnast H, Maybody M, Getrajdman GI, Bains MS, Finley DJ, Solomon SB. Computed tomography-guided access to the cisterna chyli: introduction of a technique for direct lymphangiography to evaluate and treat chylothorax. Cardiovasc Intervent Radiol. 2011; 34:Suppl 2. S240–S244.5. Propst-Proctor SL, Rinsky LA, Bleck EE. The cisterna chyli in orthopaedic surgery. Spine (Phila Pa 1976). 1983; 8:787–792.6. Pinto PS, Sirlin CB, Andrade-Barreto OA, Brown MA, Mindelzun RE, Mattrey RF. Cisterna chyli at routine abdominal MR imaging: a normal anatomic structure in the retrocrural space. Radiographics. 2004; 24:809–817.7. Loukas M, Wartmann CT, Louis RG Jr, Tubbs RS, Salter EG, Gupta AA, et al. Cisterna chyli: a detailed anatomic investigation. Clin Anat. 2007; 20:683–688.8. Williams PL, Bannister LH, Berry MM. Cardiovascular system. Gray's anatomy. 38th ed. New York: Churchill Livingstone;1995. p. 1609–1611.9. Erden A, Fitoz S, Yagmurlu B, Erden I. Abdominal confluence of lymph trunks: detectability and morphology on heavily T2-weighted images. AJR Am J Roentgenol. 2005; 184:35–40.10. Guyton AC, Hall JE. The microcirculation and the lymphatic system. Textbook of medical physiology. 9th ed. Philadelphia: Saunders;1996. p. 162–173.11. Rosenberger A, Abrams HL. Radiology of the thoracic duct. Am J Roentgenol Radium Ther Nucl Med. 1971; 111:807–820.12. Helzel MV. [Sonographic imaging of the ascending lumbar vein and the cisterna chyli or lumbar trunks]. Rofo. 1984; 140:172–174.13. Koslin DB, Stanley RJ, Berland LL, Shin MS, Dalton SC. Hepatic perivascular lymphedema: CT appearance. AJR Am J Roentgenol. 1988; 150:111–113.14. Feuerlein S, Stolz J, Muche R, Hetzel M, Klass O, Brambs HJ, et al. Cisterna chyli in patients with malignancy-Influence of cardiovascular disease on the prevalence of the cisterna. Eur J Radiol. 2011; 79:262–265.15. Deimer EE. Lymphatic anatomy. In : Herlinger H, Lunderquist A, Wallace S, editors. Clinical radiology of the liver. New York: Dekker;1983. p. 55–63.16. Takahashi H, Kuboyama S, Abe H, Aoki T, Miyazaki M, Nakata H. Clinical feasibility of noncontrast-enhanced magnetic resonance lymphography of the thoracic duct. Chest. 2003; 124:2136–2142.17. Zironi G, Cavalli G, Casali A, Piscaglia F, Gaiani S, Siringo S, et al. Sonographic assessment of the distal end of the thoracic duct in healthy volunteers and in patients with portal hypertension. AJR Am J Roentgenol. 1995; 165:863–866.18. Kedar RP, Cosgrove DO. Echo-poor periportal cuffing: ultrasonographic appearance and significance. J Clin Ultrasound. 1993; 21:464–467.19. Matsui O, Kadoya M, Takashima T, Kameyama T, Yoshikawa J, Tamura S. Intrahepatic periportal abnormal intensity on MR images: an indication of various hepatobiliary diseases. Radiology. 1989; 171:335–338.20. Abrams HL, Baum S, Pentecost MJ. Abrams' angiography: vascular and interventional radiology. vol. 2:4th ed. Boston: Little, Brown and Company;1997. p. 1891–1906.21. Feuerlein S, Kern M, Muche R, Ernst AS, Juchems MS, Pauls S. Cisterna chyli in patients with malignancy--is there a correlation between changes in cisterna volume and progression or regression of the tumor? Eur J Radiol. 2010; 76:177–179.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left-Sided Cisterna Chyli: a Case Report on a Rare Normal Anatomic Structure
- Abdominal Organ Injuries with Chyloperitoneum after Blunt Tauma: A Case Report
- Clinical significance of mega cisterna magna
- The Mega Cisterna Magna: Report of 4 Cases
- A Case of Cysticercosis Cellulosae in Cisterna Magna Diagnosed by CT Scan