J Korean Soc Radiol.
2011 Dec;65(6):555-562. 10.3348/jksr.2011.65.6.555.
Factors Affecting Longevity of Tunneled Central Venous Catheters
- Affiliations
-
- 1Department of Radiology, Kyungpook National University Hospital, Daegu, Korea. jonglee@knu.ac.kr
- KMID: 2002921
- DOI: http://doi.org/10.3348/jksr.2011.65.6.555
Abstract
- PURPOSE
To evaluate factors which affect the longevity of tunneled central venous catheters (T-CVCs).
MATERIALS AND METHODS
A retrospective study was conducted on 363 T-CVCs. We evaluated the relevant factors affecting the longevity of the T-CVCs, such as age, gender, indication for catheterization, site of entry vessel, diameter and type of T-CVC, catheter tip position, and underlying diseases.
RESULTS
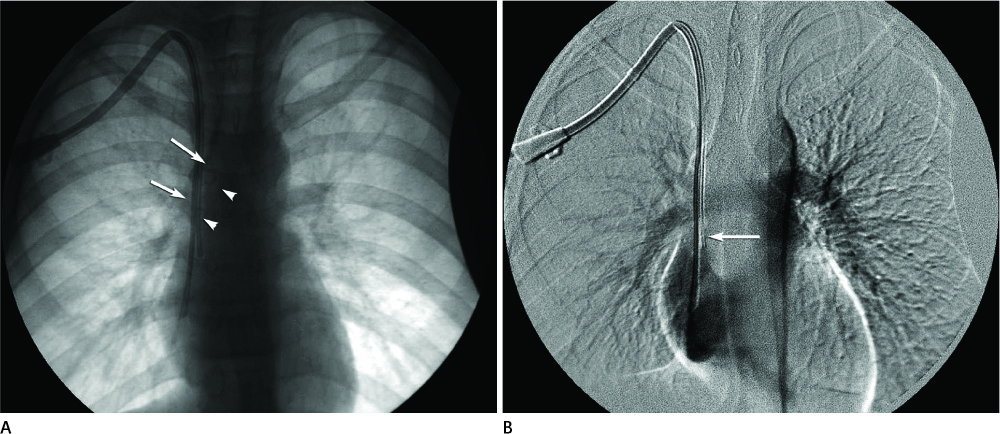
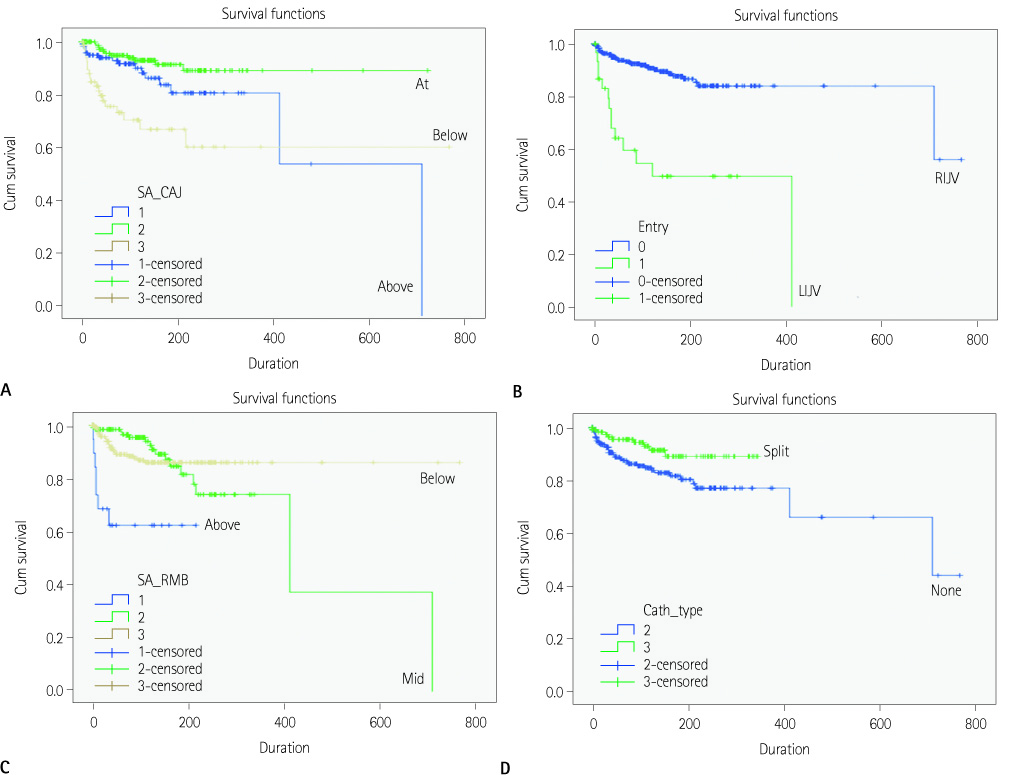
Of the 363 T-CVCs which had been inserted, 331 (91%) were placed through the right internal jugular vein (RIJV). The catheter tip position was the strongest predictor for the longevity of the T-CVC. The short limb of the catheter tip placed either at the cavoatrial junction (CA junction) or below the lower margin of the right main bronchus had a good prognosis. The vessel through which the T-CVC was placed significantly influenced the longevity of the T-CVC; the RIJV was associated with better results than the left internal jugular vein. Also, a split-type catheter was significantly associated with a better result.
CONCLUSION
A two distinct and separate type T-CVC placed through the RIJV in which the short limb catheter tip position was at the level of the CA junction, significantly increased the longevity of T-CVCs.
MeSH Terms
Figure
Reference
-
1. Ash SR. Advances in tunneled central venous catheters for dialysis: design and performance. Semin Dial. 2008; 21:504–515.2. O'Dwyer H, Fotheringham T, O'Kelly P, Doyle S, Haslam P, McGrath F, et al. A prospective comparison of two types of tunneled hemodialysis catheters: the Ash Split versus the PermCath. Cardiovasc Intervent Radiol. 2005; 28:23–29.3. Robertson LJ, Mauro MA, Jaques PF. Radiologic placement of Hickman catheters. Radiology. 1989; 170:1007–1009.4. Fry AC, Stratton J, Farrington K, Mahna K, Selvakumar S, Thompson H, et al. Factors affecting long-term survival of tunnelled haemodialysis catheters--a prospective audit of 812 tunnelled catheters. Nephrol Dial Transplant. 2008; 23:275–281.5. Quarello F, Forneris G, Borca M, Pozzato M. Do central venous catheters have advantages over arteriovenous fistulas or grafts? J Nephrol. 2006; 19:265–279.6. Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006; 48:Suppl 1. S176–S247.7. Petersen J, Delaney JH, Brakstad MT, Rowbotham RK, Bagley CM Jr. Silicone venous access devices positioned with their tips high in the superior vena cava are more likely to malfunction. Am J Surg. 1999; 178:38–41.8. Charvát J, Linke Z, Horáèková M, Prausová J. Implantation of central venous ports with catheter insertion via the right internal jugular vein in oncology patients: single center experience. Support Care Cancer. 2006; 14:1162–1165.9. Darling JC, Newell SJ, Mohamdee O, Uzun O, Cullinane CJ, Dear PR. Central venous catheter tip in the right atrium: a risk factor for neonatal cardiac tamponade. J Perinatol. 2001; 21:461–464.10. Dillon MF, Curran J, Martos R, Walsh C, Walsh J, Al-Azawi D, et al. Factors that affect longevity of intravenous cannulas: a prospective study. QJM. 2008; 101:731–735.11. Kröger K, Ose C, Rudofsky G, Roesener J, Weiland D, Hirche H. Peripheral veins: influence of gender, body mass index, age and varicose veins on cross-sectional area. Vasc Med. 2003; 8:249–255.12. Yang F, Minutello RM, Bhagan S, Sharma A, Wong SC. The impact of gender on vessel size in patients with angiographically normal coronary arteries. J Interv Cardiol. 2006; 19:340–344.13. Jacobson AF, Winslow EH. Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung. 2005; 34:345–359.14. Maki DG, Ringer M. Risk factors for infusion-related phlebitis with small peripheral venous catheters. A randomized controlled trial. Ann Intern Med. 1991; 114:845–885.15. Haddad FG, Waked CH, Zein EF. Peripheral venous catheter-related inflammation. A randomized prospective trial. J Med Liban. 2006; 54:139–114.16. Cornely OA, Bethe U, Pauls R, Waldschmidt D. Peripheral Teflon catheters: factors determining incidence of phlebitis and duration of cannulation. Infect Control Hosp Epidemiol. 2002; 23:249–253.17. Uslusoy E, Mete S. Predisposing factors to phlebitis in patients with peripheral intravenous catheters: a descriptive study. J Am Acad Nurse Pract. 2008; 20:172–180.18. Malach T, Jerassy Z, Rudensky B, Schlesinger Y, Broide E, Olsha O, et al. Prospective surveillance of phlebitis associated with peripheral intravenous catheters. Am J Infect Control. 2006; 34:308–312.19. Monreal M, Quilez F, Rey-Joly C, Rodriguez S, Sopena N, Neira C, et al. Infusion phlebitis in patients with acute pneumonia: a prospective study. Chest. 1999; 115:1576–1580.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Insertion and Management of Central Venous Catheters
- Radiologic Placement of Tunneled Central Venous Catheters in Pediatric Patients
- Comparison of Step Tip Type and Split Tip Type Hemodialysis Catheter: HemoGlide Versus the HemoSplit
- Association between initial vascular access and survival in hemodialysis according to age
- Analysis of the Outcome of Tunneled Hemodialysis Catheters in Children according to the Indications for Use