J Korean Soc Radiol.
2013 Nov;69(5):365-371. 10.3348/jksr.2013.69.5.365.
Paragonimiasis: A Pictorial Essay
- Affiliations
-
- 1Department of Radiology, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea. ksbae@gnu.ac.kr
- 2Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Department of Thoracic Surgery, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- 4Department of Pathology, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2002857
- DOI: http://doi.org/10.3348/jksr.2013.69.5.365
Abstract
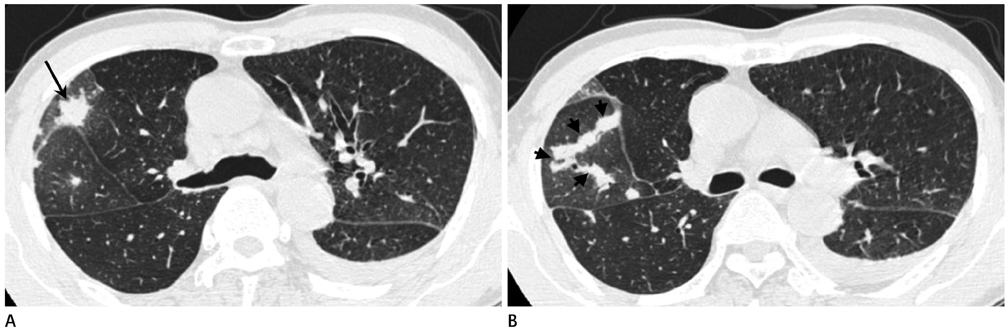
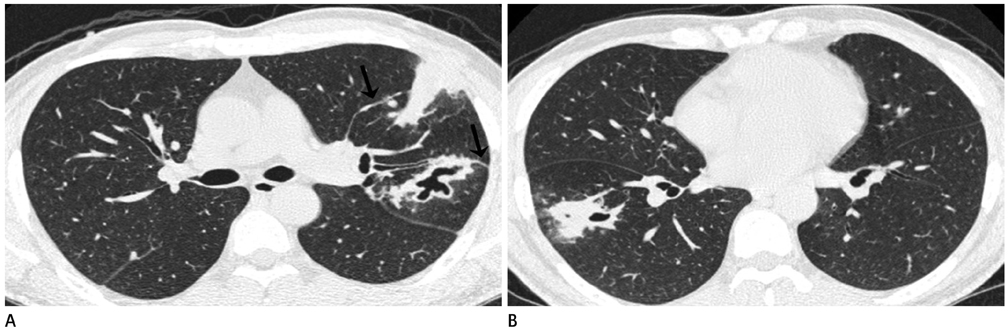
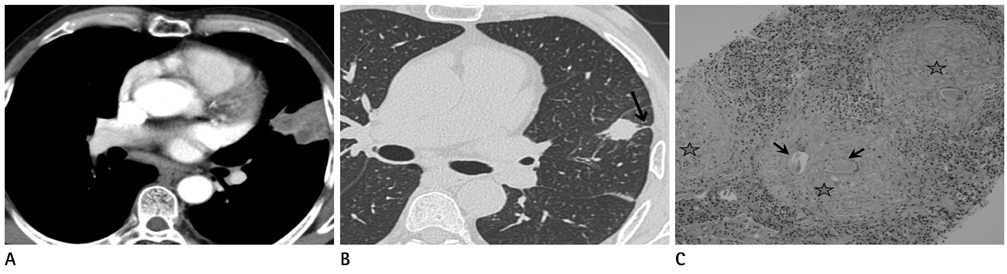
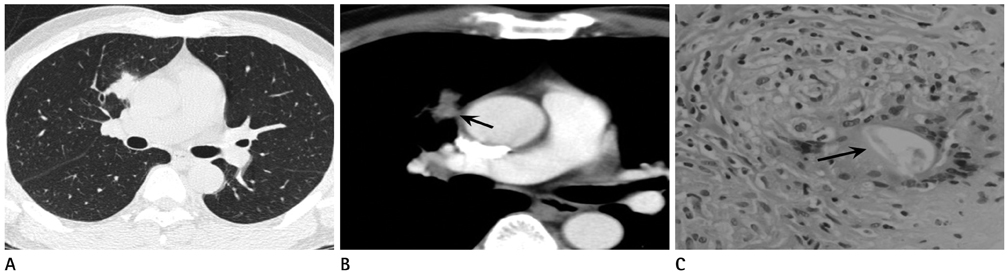
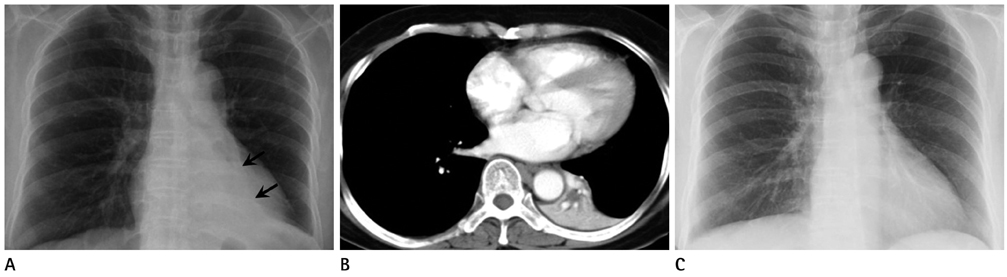
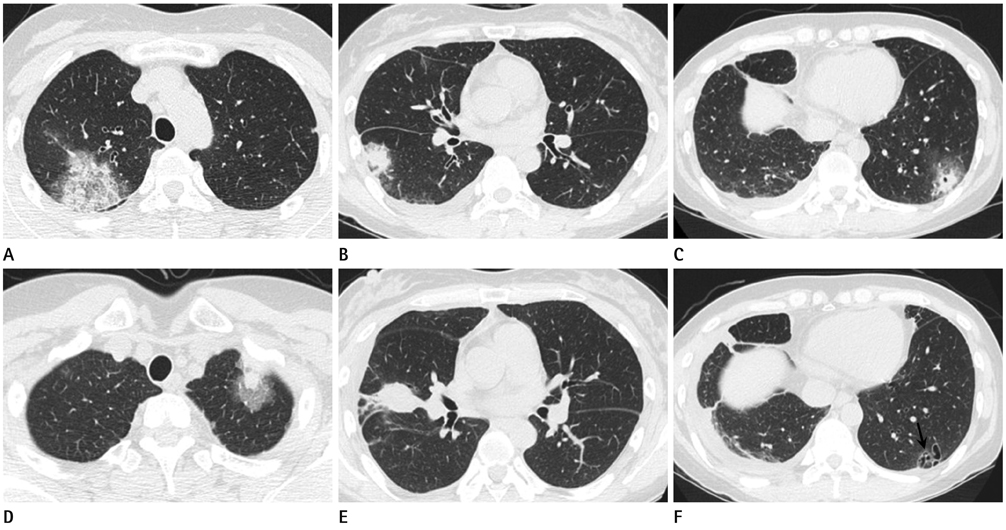
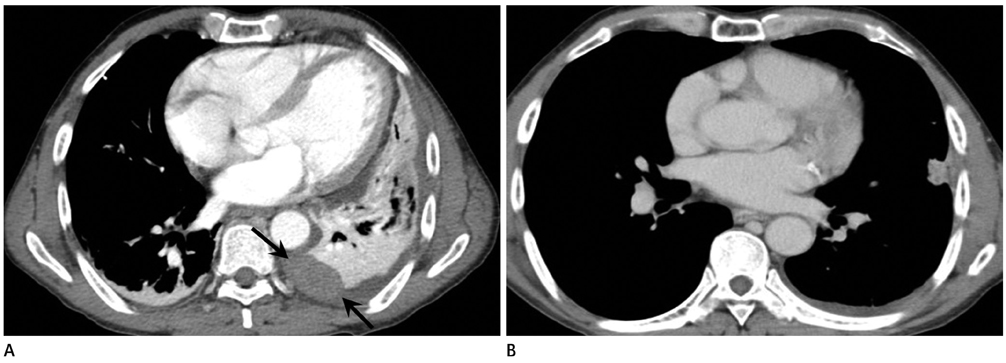
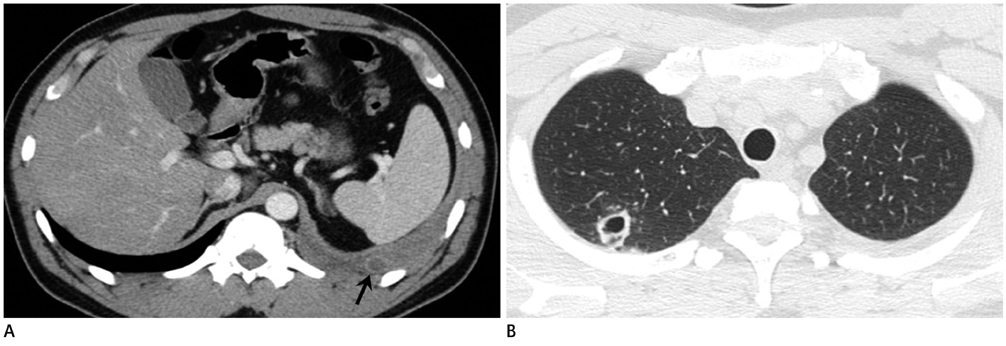
- Pleuropulmonary paragonimiasis is a parasitic infection caused by lung flukes including Paragonimus westermani. Paragonimiasis usually occurs from ingestion of raw or improperly cooked freshwater crabs or crayfish. Pleural or lung parenchymal lesions are commonly found on CT or chest radiographs, and radiologic manifestations of pleuropulmonary paragonimiasis vary with the stage of the disease. Early findings include pneumothorax or hydrothorax, focal air-space consolidation, and linear opacities. Later findings include thin-walled cysts, mass-like consolidation, nodules, or bronchiectasis. Pulmonary paragonimiasis often can be mistaken for pulmonary tuberculosis in tuberculosis-endemic areas or lung cancer when it presents as a solitary pulmonary nodule. Intraperitoneal or ectopic lesions such as those in the retroperitoneum can form during migration of a juvenile worm from the small intestine to the lungs. Although the symptoms and signs of pulmonary paragonimiasis are nonspecific, an early diagnosis can be made if radiologists understand the pathogenesis and typical imaging findings of the disease. The purpose of this report was to demonstrate the various imaging findings of pleuropulmonary paragonimiasis and to review articles to help radiologists make a proper diagnosis.
MeSH Terms
Figure
Cited by 2 articles
-
Pulmonary Paragonimiasis Misdiagnosed with Pulmonary Tuberculosis
Su Eun Park, Bokyung Song, Jae-Yeon Hwang
Pediatr Infect Vaccine. 2017;24(3):178-182. doi: 10.14776/piv.2017.24.3.178.Status of common parasitic diseases in Korea in 2019
Sun Huh
J Korean Med Assoc. 2019;62(8):437-456. doi: 10.5124/jkma.2019.62.8.437.
Reference
-
1. Choi DW. Paragonimus and paragonimiasis in Korea. Korean J Parasitol. 1990; 28:Suppl. 79–102.2. Choi WY, Lee OR, Jin YK, Chi JG. [Lung findings in experimental Paragonimiasis]. Korean J Parasitol. 1979; 17:132–146.3. Im JG, Kong Y, Shin YM, Yang SO, Song JG, Han MC, et al. Pulmonary paragonimiasis: clinical and experimental studies. Radiographics. 1993; 13:575–586.4. Song JU, Um SW, Koh WJ, Suh GY, Chung MP, Kim H, et al. Pulmonary paragonimiasis mimicking lung cancer in a tertiary referral centre in Korea. Int J Tuberc Lung Dis. 2011; 15:674–679.5. Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS, Lee KS, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005; 128:1423–1430.6. Im JG, Whang HY, Kim WS, Han MC, Shim YS, Cho SY. Pleuropulmonary paragonimiasis: radiologic findings in 71 patients. AJR Am J Roentgenol. 1992; 159:39–43.7. Kim TS, Han J, Shim SS, Jeon K, Koh WJ, Lee I, et al. Pleuropulmonary paragonimiasis: CT findings in 31 patients. AJR Am J Roentgenol. 2005; 185:616–621.8. Kim SY, Ha HK. Peritoneal manifestations of parasitic infection. Abdom Imaging. 2008; 33:172–176.9. Shim SS, Kim Y, Lee JK, Lee JH, Song DE. Pleuropulmonary and abdominal paragonimiasis: CT and ultrasound findings. Br J Radiol. 2012; 85:403–410.10. Lee CH, Kim JH, Moon WS, Lee MR. Paragonimiasis in the abdominal cavity and subcutaneous tissue: report of 3 cases. Korean J Parasitol. 2012; 50:345–347.11. Jeong MG, Yu JS, Kim KW, Kim JK, Kim SJ, Kim HJ, et al. Retroperitoneal paragonimiasis: a case of ectopic paragonimiasis presenting as periureteral masses. J Comput Assist Tomogr. 1999; 23:696–698.12. Kong Y, Cho SY, Han MH, Goo JM, Yu IK, Shin YM, et al. An experimental study on cerebral paragonimiasis using cats. J Korean Radiol Soc. 1994; 30:1003–1012.13. Oh IJ, Kim YI, Chi SY, Ban HJ, Kwon YS, Kim KS, et al. Can pleuropulmonary paragonimiasis be cured by only the 1st set of chemotherapy? Treatment outcome and clinical features of recently developed pleuropulmonary paragonimiasis. Intern Med. 2011; 50:1365–1370.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pictorial, Essay : Sonography of the Stomach
- Multi-Detector CT Findings of Typical and Atypical Appendicitis: A Pictorial Essay
- Unusual, but important, peri- and extra-articular manifestations of rheumatoid arthritis: a pictorial essay
- Breast lesions during pregnancy and lactation: a pictorial essay
- CT Findings of Central Airway Lesions Causing Airway Stenosis-Visualization and Quantification: A Pictorial Essay